Pelvic health after having my baby
► Perineal wound care
It is really important to keep your perineum (the area between your vagina and back passage) as clean and dry as you can. Use water to wash especially after any tears or stitches as this helps to reduce infection and promote healing. It is not advised to use soap or shower gel as this can increase irritation and skin sensitivity. Pat the area dry rather than wiping or rubbing. Avoid long hot baths until your stitches have healed – 2 weeks minimum.
Pain and swelling can last 7-14 days after having a baby. Using pain medication as advised or using a cold pack can help.
Some positions are often more comfortable – lying on your side or sitting with a pillow under your thighs – to reduce pressure on your perineum/stitches.
Perineal Care Patient Information Leaflet
Looking after your pelvic floor when you have had a baby (mkuh.nhs.uk)
► Discomfort or pain with sex
Sometimes a change in the tissue due to stretching can make the vaginal area feel stretched or loose or even that ‘something is in the way’. Discomfort can sometimes be due to scar tissue from healing after a tear or an episiotomy. Altered sensation can happen – increasing sensitivity or reducing it, due to involvement in the nerves in the area which may have been stretched or bruised.
It is safe to resume sex around 6 weeks after delivery as long as any wounds have healed, and you feel comfortable and ready. It may help to use a water-based lubricant especially if you are breastfeeding as this can cause some vaginal dryness.
If you notice any signs of infection – foul smelling discharge, excessive itching, increased pain or swelling – you should contact your midwife or GP for advice.
However, if after 6-12 weeks following delivery, you continue to feel pain for no obvious reason, please speak to your GP and ask for a referral to Pelvic Health physiotherapy.
► Bladder care
The pelvic floor is important for bladder and bowel control and for increase satisfaction during sex. Weak pelvic floor muscles do not support the pelvic organs correctly, which along with bladder and bowel weakness, can lead to prolapse (dropping of the uterus, bladder or bowel).
The first 24 hours after the birth
- Empty your bladder every couple of hours. The feeling of wanting to pass urine may not return straight away. You must tell your midwife if you are unable to empty your bladder within six hours following delivery.
- Do short pelvic floor muscle squeezes at first. It will help any swelling to go down and can help to heal tears and stitches. Lying on your side is a comfortable position to start exercising.
- Keep the perineum clean and dry until healed using only warm water to wash. Do not use any creams, gels or soap in the area as they can cause infection and irritation to new skin. Stitches should dissolve within 10-14 days – discomfort should reduce daily. If not, please ask your midwife or GP to check them at your post-natal appointments.
- Use medication as advised by your midwife or doctor if your perineum (the area between the vagina and back passage) is uncomfortable. This will help to keep you mobile, which in turn helps the healing process.
- Refer to the Perineal care booklet provided on the ward.
- You could also try using an ice-pack – this will help to reduce swelling and discomfort and ease bruising. When you are at home you can use a damp frozen pantyliner or a ready-made gel ice pack in a damp clean flannel and placing it on the perineum (the area between the vagina and anus) for 5 minutes, while you are lying down. Do not sit on it.
Caution: ice can burn so do not leave it in place for longer than five minutes.
- If you have difficulty controlling your bladder or bowels after delivery please ask your GP /Midwife to refer you to Women’s Health physiotherapy. You may feel worried about emptying your bowels for the first time.
- Using a wad of toilet paper or maternity pad, support the area just in front of your back passage to support it while you gently bear down with a series of short pushes (rather than straining).
You must tell your midwife if:
- you can’t pass any wee or
- if there is no sensation to need to wee or
- you are leaking wee when you stand or move around
► Pelvic floor exercises
The pelvic floor muscle group is like a hammock stretched across the base of the pelvis. There are three openings in the muscle – the anus (back passage), vagina (birth canal) and urethra (bladder outlet).
Sit comfortably or lie on your side
Imagine that you are trying to stop yourself passing urine and ‘wind’, by drawing the area ‘upwards and forwards’ from bowel to bladder, then let go. Start this ‘squeezing and lifting’ movement gently at first. Next ‘squeeze and lift’ and try to hold for a few seconds (breathe normally –don’t hold your breath and ensure your buttocks and thighs are relaxed!). This is a ‘slow hold’.
Rest for a moment and then repeat four times if you can.
Now try squeezing the pelvic floor muscles quickly five times, with a little rest between each squeeze. This exercise helps your muscles react quickly when you cough or sneeze. Try five ‘slow hold’ squeezes, followed by five ‘quick’ squeezes at least four times a day. As your muscles get stronger, try holding the ‘slow’ holds for longer.
Don’t stop and start your flow of urine – this can interfere with normal bladder function.
Use the NHS-approved ‘Squeezy’ App available on all smart phones/mobile devices to help remind you to complete exercises using the exercise plan described above.
Getting back to normal
- Do your pelvic floor exercises regularly. The hardest part is remembering to do them – a good time could be every time you feed your baby or wash your hands.
- Tighten your pelvic floor when you do any activity that requires effort – e.g. cough, sneeze or lift. The reflex that makes you do this naturally can stop working after having a baby. Regular practice protects your pelvic floor and helps to train it to work automatically again.
- Avoid heavy lifting where possible – e.g. vacuuming, wet washing, car seats.
- Avoid sit ups and high impact exercise for at least 3 months after the birth – it can take the pelvic floor this long or more to return to its previous pre-natal strength.
- Drink at least 1.5 – 2 litres of fluid a day, which is about six to eight drinks. If you are breast-feeding or it is very hot you should maintain good hydration by drinking according to your thirst and ensuring that you have lightly coloured urine.
- Avoid constipation – it puts pressure on the pelvic floor.
- Once your pelvic floor muscles are back to full strength, you will need to do one set of ‘fast’ and ‘slow’ exercises every day to keep them strong. Aim for 10 fast and 10 slow holds for 10 seconds.
Click here for further advice and safe exercises
Are you at risk of developing pelvic floor problems?
- Did you have urinary leakage in pregnancy?
- Did you struggle with continence – bladder or bowel post-natally?
- Does/ did your mother have continence or prolapse problems?
- Did you have a large baby (over 4kgs) or an instrumental (forceps/ventouse) delivery?
- Did you have a very long or very fast ‘pushing’ (second) stage of labour?
- Do you suffer regularly from constipation?
► Recovering after Caesarean Section
First Day
Breathing Exercises, in sitting or lying
Bend your knees up a little if you are lying down. Take a deep breath in through your nose, hold for two seconds, then sigh out. Be aware of your lower ribs expanding as you breathe in. Repeat three to four times.
Coughing
You may produce phlegm which needs clearing, particularly if you smoke. Support your stitches with your hands or a rolled up towel, take a deep breath, then ‘huff’ – a hard, forceful breath out. Follow this with a cough. You will not harm your stitches by coughing, and discomfort is reduced if you support your stitches.
Circulation exercises
While you are not walking about it is important to maintain blood flow in your legs to prevent a clot forming. Bend your feet up and down from the ankle briskly 15 times. You can also circle the ankles.
Circulation and breathing exercises should be done every hour.
Turning over and getting out of bed
Before moving, bend your knees up and draw in the lower part of your tummy a small amount to ‘brace’ it. Reach your arm over in the direction you want to go, at the same time roll your knees over.
To get out of bed, drop your legs over the side and push yourself up in to sitting.
Standing up – put your hands on the side of the bed, draw in your lower tummy muscles, lean forward and push yourself up into standing. Remember to ‘stand tall’ when you walk.
Going to the toilet
You will have a catheter at first to drain your bladder. Sometimes the normal bladder sensations take a little while to return to normal after it is removed. After the catheter is removed, don’t leave it longer than three hours before you try to pass urine as it is important that your bladder doesn’t overfill. Take your time, to make sure that your bladder is completely empty. Tell your midwife if you are unable to pass urine.
Pelvic Floor exercises
Even though you have not had a vaginal delivery, your pelvic floor muscles have been supporting the weight of your baby throughout your pregnancy, so you need to exercise them to help recover their strength. The pelvic floor is a group of muscles like a hammock at the base of the pelvis. It has three openings – the urethra (the bladder outlet), the vagina (birth canal) and the anus (back passage). It supports the pelvic organs and helps control the bladder and bowels.
When your catheter has been removed, you can start these exercises
Sit comfortably or lie on your side. Imagine that you are trying to stop yourself passing urine and ‘wind’, by ‘squeezing and lifting’ the openings of the bladder and bowels, then let go. Start gently at first. ‘Squeeze and lift’ and try to hold for a few seconds (breathe normally –don’t hold your breath!) This is a ‘slow hold’. Rest for a moment, and then repeat five times if you can.
Now try squeezing the pelvic floor muscles quickly five times, with a little rest between each squeeze. This exercise helps your muscles react quickly when you cough or sneeze.
How often do you need to exercise your pelvic floor muscles?
• Try five ‘slow hold’ squeezes, followed by five ‘quick’ squeezes at least four times a day
• As your muscles get stronger, try holding the ‘slow’ holds for longer
• The hardest part is remembering to do your pelvic floor exercises – a good time to do them is every time you feed your baby
• Do not stop and start your flow of urine – this can interfere with normal bladder function.
You can download the NHS approved Squeezy app to help remind you to do pelvic floor exercises.
An early tummy exercise – You can start this on the first day, if you feel ready.
Sitting
Support the lower part of your tummy with your hands or a towel. Squeeze and lift the pelvic floor, at the same time draw in the lower part of your tummy a small amount. Hold for three seconds while you breathe out. Relax, then repeat five times. Gradually increase the time you hold the muscle in. Bracing these muscles as you change position, get up from the chair or bed, or pick up your baby will help to make these movements more comfortable.
How to progress your exercises
After a couple of days you can move on to the exercises in the leaflet ‘Getting back into shape after your delivery’. Take your exercises at a steady pace, and don’t try to progress too quickly, particularly with strong tummy exercises. Your scar will heal quickly, but it takes several weeks for the deep muscles and the scar on the uterus to become strong.
Going home
You will need to rest at home, but continue with your exercises twice a day, gradually increasing the repetitions as you get stronger. Once your pelvic floor muscles are back to full strength, you will need to do a set of ‘fast’ and ‘slow’ exercises every day to keep them strong.
Walking for a short distance each day will improve your fitness and strengthen your muscles. Start gently with a five minute walk at a steady pace, building up the distance and the pace at which you walk as you recover. Avoid lifting, where possible, until you are six weeks post-natal.
If you continue to have pain from caesarean section scar after six weeks ask your GP to refer you to our experienced Women’s Health Physiotherapy team at MKUH. If you experience any problems with bladder control you can self-refer directly on 01908 995 432.
► Your stomach muscles
► Return to exercise
You will want to give your baby lots of attention, but it is also important to find time for yourself. By regaining your fitness, you will feel good and have more energy. You may also prevent some health problems in the future. You can start gentle exercises from day one if you feel ready. Start gently and build up.
Pelvic Floor exercises
The pelvic floor is a group of muscles like a hammock at the base of the pelvis. It has three openings – the urethra (the bladder outlet), the vagina (birth canal) and the anus (back passage). It supports the pelvic organs and helps prevent leaking from the bladder and bowels. Your pelvic floor will probably feel very weak after your delivery, so it is important to start your exercises within the first day or two to help it regain its strength.
If you have a catheter wait until it is removed before starting your pelvic floor exercises.
If you have stitches you can still do these exercises – they will help healing by reducing swelling in the area – but start gently.
Using ice wrapped in a damp flannel may help reduce swelling & pain and promote healing – used for five minutes every hour.
Sit comfortably or lie on your side. Imagine that you are trying to stop yourself passing urine and ‘wind’, draw the area upwards and forwards from bowel to bladder – then let go. Start this ‘squeezing and lifting’ movement gently at first. Then ‘squeeze and lift’ and try to hold for a few seconds (breathe normally – don’t hold your breath!). This is a ‘slow hold’. Rest for a moment, and then repeat five times if you can.
Now try squeezing the pelvic floor muscles quickly five times, with a little rest between each squeeze. This exercise helps your muscles react quickly when you cough or sneeze – preventing urinary leakage and pressure on your stitches. Try five ‘slow hold’ squeezes, followed by five quick squeezes at least four times a day. As your muscles get stronger, try holding the ‘slow’ holds for longer – aim for 10 slow holds for 10 secs and 10 fast contractions. It can take several months of regular exercises for the pelvic floor to return to its previous strength.
The hardest part is remembering to do your pelvic floor exercises – a good time to do them is every time you feed your baby. Or try the NHS ‘Squeezy’ App – available on all mobile devices to get into a lifetime routine of regular exercises – set the exercise plan with programme above to start with.
Don’t stop and start your flow of urine – this can interfere with normal bladder function.
Exercises for the tummy muscles
Day One
Sitting or lying on your side, place your hand on the lower part of your tummy, to feel your muscles working. Squeeze and lift the pelvic floor, at the same time draw in the lower part of your tummy a small amount, away from your hand. Hold for three seconds while you breathe out. Relax, and then repeat five times. Gradually increase the time you hold the muscle in.
Once you are happy with these exercises, try holding these muscles in a small amount when you are walking about, rather than letting them ‘sag’ – walking tall. Then remember to tighten them during any activity that requires effort – e.g. lifting or changing your baby.
More early exercises
You can add these when you feel ready, from Day two.
Lying down bend your knees up. Brace the pelvic floor and tummy muscles as Day one exercise, then allow your knees to roll to the right as far as is comfortable. Bring them back to the centre, and then repeat to the left. Try three times to each side. Bend your knees up. Tighten the pelvic floor, then hollow your tummy and flatten your back into the bed and allow your ‘tail’ to tilt upwards. Hold for three seconds, then gently release. Repeat four times.
Exercises to avoid
- Do not try full sit-ups until your tummy muscles are strong.
- Never do ‘double straight leg lifts’ as these can damage your back and the pelvic floor muscles.
- Always tighten your pelvic floor muscles first before doing any tummy exercise.
Your deep tummy muscles and pelvic floor are also important in protecting your back from injury.
As you will be doing lots of lifting in the next few months, work on improving their strength.
[section=General advice]
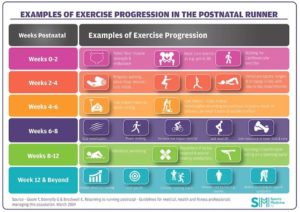
6-12 weeks postnatal
- It is important to ensure your vaginal bleeding has stopped and your caesarean section or perineal wound is healed.
- Start building exercise with low impact exercise before gradually building endurance, strength and intensity –
- Pilates/yoga
- Swimming or cycling
- Cross training or power walking
- Light weights
After 12 weeks
- You can start to build your programme doing cardio and muscle strength training by
- Increasing the weights slowly
- Increasing the length of exercise session
- Introducing higher impact training – jogging, running, HIIT or zumba
► Self-referral
Any change in exercise should be comfortable and not cause or increase any symptoms of pelvic floor dysfunction or bulging of the tummy muscles. If you have any concerns stop immediately and ask your GP for a referral to pelvic health physio. Or self refer for UI:
► Resources
Last Modified: 2:23pm 17/10/2023
