Antenatal Checks
It is very important to attend antenatal and scan appointments that are made for you during your pregnancy. If you cannot attend any appointments, please contact your Midwife or the hospital to re-arrange.
Your Midwife or Doctor will check you and your baby’s health and wellbeing at each of these appointments. Please discuss any worries or questions that you may have. If you have had any tests or investigations, make sure that you ask for the results at your next appointment.
This is checked to detect pregnancy induced hypertension or pre-clampsia. High blood pressure may cause severe headaches or flashing lights. If this happens, tell your Midwife or Doctor immediately.► Blood pressure
You will be asked to supply a sample of your urine at each visit to check for protein (recorded as + or ++= presence of), which may be a sign of pre-eclampsia and glucose which may be a sign of gestational diabetes.► Urine tests
You will usually start feeling some movements between 16 and 24 weeks. A baby’s movements can be described as anything from a kick, flutter, swish or roll. You will very quickly get to know the pattern of your baby’s movements. At each antenatal contact your Midwife will talk to you about this pattern of movements which you should feel each day up to the time you go into labour and whilst you are in labour too. Become familiar with your baby’s usual daily pattern of movements and contact your Midwife or Maternity Unit immediately if you feel that the movements have altered. Do not put off calling until the next day. It is important for your doctors and midwives to know if your baby’s movements have slowed down or stopped. A change, especially slowing down or stopping, can sometimes be an important warning sign that the baby is unwell and the baby needs checking by ultrasound and Doppler. If, after your check up, you are still not happy with your baby’s movements, you must contact either your Midwife or Maternity Unit straight away, even if everything was normal last time. Never hesitate to contact your Midwife or the Maternity Unit for advice, no matter how many times this happens.► Fetal movements
If you wish your Midwife or Doctor can listen to the baby’s heart with either a stethoscope or a fetal Doppler. With a Doppler you can hear the heartbeat yourself. The use of home fetal Dopplers to listen to your baby’s heartbeat is not recommended. Even if you detect a heartbeat this does not mean your baby is well and you may be falsely reassured.► Fetal heart (FH or FHHR – fetal heart heard and regular)
► Liquor
This refers to the amniotic fluid which is the water around the baby. A gentle examination of the abdomen can give an idea of whether the amount is about right (recorded as NAD – no abnormality detected or just N), or whether there is suspicion of there being too much or too little, in which cases an ultrasound is needed.
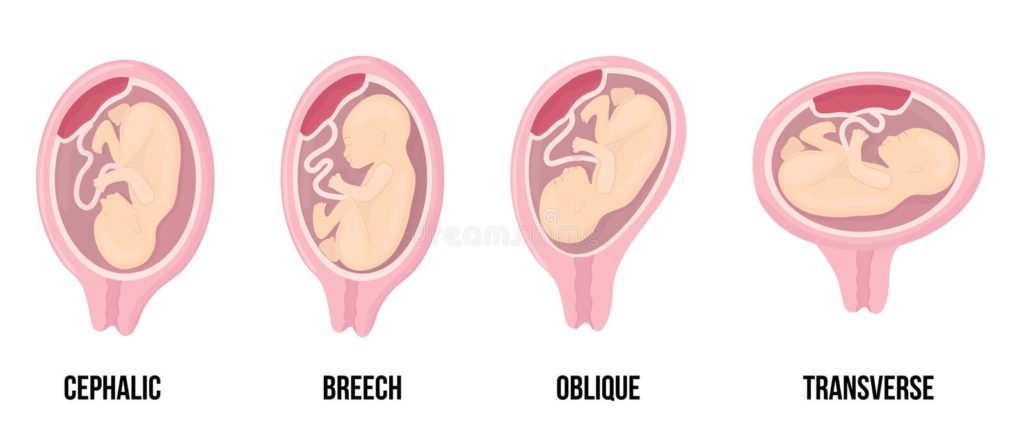
► Lie and presentation
This describes the way the baby lies in the womb (L = longitudinal; O = oblique; T = transverse) and which part it presents towards the birth canal (head first = C; bottom first = B or Br).
This is how deep the presenting part e.g. the baby’s head is below the brim of the pelvis/ It is measured by how much can be felt through the abdomen in fifths )e.g., 5/5 = free; 3/5 = lower but most is still above the brim; 1/5 or 0/5 = deeply engaged, as hardly still felt from above). In first time mothers, engagement tends to happen in the last weeks of pregnancy. In subsequent pregnancies, it may occur later, or not until labour has commenced.► Engagement
► Assessing fetal growth
Accurate assessment of the baby’s growth inside the womb is one of the key tasks of good antenatal care. Problems such as growth restriction can develop unexpectedly and is liked with a significantly increased risk of adverse outcomes including stillbirths, fetal distress during labour, neonatal problems or cerebral palsy. Therefore it is essential that the baby’s growth is monitored carefully.
Fundal height is measured every 2-3 weeks from 26-28 weeks onwards, ideally by the same Midwife or Doctor. The measurements are taken with a centimetre tape from the fundus (top of the uterus) to the top of the symphysis (pubic bone) and then plotted on the growth chart. The slope of the measurements should be similar to the slope of the three curves printed on the chart which predict the optimal growth of your baby.
Customised growth charts – these notes have been developed to support the use of customised growth charts which are individually adjusted for you and your baby. The information required included:
- your height and weight in early pregnancy
- your ethnic origin
- number of previous babies, their name, sex, gestation at birth and birthweight
- the expected date of delivery (EDD) which is usually calculated from the dating ultrasound
The chart is created after your pregnancy dates have been determined by ultrasound (preferably) or by last menstrual period. If neither dates are available, regular ultrasound scans are recommended to check that the baby is growing as expected. If you wish to have access to the chart, please ask your midwife. For further information about customised growth charts click here.
Growth restriction – slow growth is one of the most common problems that can affect the baby in the womb. If the fundal height measurements suggest there is a problem, an ultrasound scan should be arranged and the estimated fetal weight (degree of error 10-15%) should be plotted on the customised chart to assess whether the baby is small for gestational age. If it does record as small, an assessment of Doppler flow is recommended. This assessment indicated how well the placenta is managing the blood supply needed for the baby. If there is a serious problem, your Obstetric team will need to discuss with you the best time to deliver the baby.
Large baby (macrosomia) – sometimes the growth curve is larger than expected. A large fundal height measurement is usually no cause for concern, but if the slope of subsequent measurements is too steep, your carers may refer you for an ultrasound scan to check the baby and the amniotic fluid volume. Big babies may cause problems either before or during birth (obstructed labour, shoulder dystocia etc), however, most often they are born normally.
Last Modified: 4:59pm 12/10/2022
