Perineal Massage in Pregnancy – Advice and Information
Please note, this page is printable by selecting the normal print options on your computer.
Approximately 85% of women will have some degree of perineal tear or injury during vaginal delivery. Most heal without any problems or adverse effects, but for some women there may be longer term implications, this could include pain and discomfort.
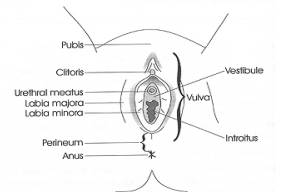
What and where is the perineum?
The perineum is an area of skin about 2-5cms which connects with the pelvic floor muscles. It is found between the vaginal opening (introitus) and the anus (back passage).
Massaging the perineum has been shown to reduce the likelihood of perineal trauma by:
- Increasing the area’s ability to stretch more easily during birth
- Reduce the need for an episiotomy
- Reduces the number of natural tears that may occur during vaginal delivery
Please note that perineal massage should only be completed from 35 weeks gestation onwards – there is no benefit in starting this before.
Women who have had a previous vaginal delivery do not experience a reduction in perineal trauma, however they do report less pain from their perineum at three months post-partum (after their baby is born).
What else can you do to prevent the likelihood of tearing your perineum?
- Upright posture such as kneeling, sitting or squatting (gravity assisted) during the second stage of labour rather than supine (lying on your back) Perineal massage
- You can ask your midwife to support your perineum as your baby is being born which reduces the risk of third- and fourth-degree tears. This is known as ‘hands on’ birth.
- You can use a warm compress on the perineum during labour – talk to your midwife about this
Discuss with your midwife if you have any further questions/concerns – for example regarding the OASI pathway
If you decide to go ahead with perineal massage, here is what you need to know:
Positions:

Supine: Patient lying on their back, head supported with pillows, with knees slightly bent.

Sitting or kneeling: Patient’s weight supported by buttocks and thighs, knees bent, feet flat on bed or floor.

Squatting: Patient’s weight on feet, knees bent.
How to massage the perineum:
- Wash your hands before and make sure your nails are short to prevent scratching the skin.
- A suitable time to do this could be during or after a warm bath or shower as this increases the blood flow to the area, which makes the perineum softer and more comfortable to touch
- We suggest using a small amount of unscented, organic oil (for example almond or olive oil) or unscented personal lubricant (e.g. Yes or Sylk) to lubricate the area and make the massage more comfortable. Do not use synthetic or scented oils (e.g. Vaseline or baby oil).
- Ensure you are in a comfortable supported position in a safe, secure environment where you are unlikely to be interrupted. You may find using a mirror helps initially. Prop yourself up with pillows to support your back in bed and bend your knees.
- Place one or both thumbs within the back wall of the vagina, resting one or both forefingers on your buttocks. Pressing down a little towards your back passage (rectum), gently massage by moving your thumb(s) and forefinger(s) together upwards and outwards then back in again.
- You should experience a stretch-like feeling which will be similar to the feeling you will have when you birth your baby. Aim to continue for 5 minutes.
- With time you will be able to apply more pressure towards your back passage as the tissue becomes more elastic and easier to relax.
- Aim to repeat 3-4x each week – or every other day.
- We recommend that you do not do perineal massage if you have thrush or vaginal herpes.
For further pictures and information on perineal massage please follow these links:
How to do perineal massage: a step-by-step guide | NCT
Antenatal perineal massage for reducing perineal trauma | Cochrane
Study findings for the effects of perineal massage:
The most recent Cochrane review of evidence looking into studies of antenatal perineal massage to prevent birth trauma (2013) found that:
- Women who performed perineal massage showed a reduction in perineal trauma requiring suturing (stitching)
- Perineal massage reduced the risk of needing an episiotomy
- Women who performed massage the most frequently were less likely to report pain
- Perineal massage is deemed as acceptable by pregnant women
- There is no increased benefit to doing perineal massage more than 3.5 times per week. We therefore recommend that you massage 3-4 times per week.
A more recent trial in 2020 concluded perineal massage reduces incidence of severe perineal trauma – Antenatal perineal massage benefits in reducing perineal trauma and postpartum morbidities: a systematic review and meta-analysis of randomized controlled trials – PubMed (nih.gov)
For further information, please visit the RCOG website.
Birth Training Devices
Birth training devices or vaginal dilatation balloons (e.g. Anibal or EPI-NO) are designed with a soft balloon which is inserted vaginally and then inflated to stretch the pelvic floor muscles in pregnancy.
There is no conclusive evidence available to suggest that birth training devices reduce the incidence of perineal trauma. Perineal massage has been proven to reduce perineal trauma and therefore we would recommend this to women from 35 weeks’ gestation.
Pelvic floor exercises
Pelvic floor exercises are important to maintain strength in the muscles supporting your baby during pregnancy to prevent problems during this period and after delivery. Doing these exercises gently after your delivery will also help improve healing postnatally. For more information, please look at our leaflet on pelvic floor exercises
Perineal healing after a vaginal birth
If you sustain any perineal trauma (including tears or episiotomy) with a vaginal birth, please visit this website for information on what to expect and things you can do to help your perineum heal.
You will also be provided with information on ‘Perineal Care’ by your midwife or physiotherapist on the postnatal ward before you are discharged.
If you have any problems with your bladder or bowel function (this can include incontinence of urine or poo, leakage of wind, urgency or frequency); have any symptoms of prolapse, scar pain or are struggling to return to sexual intercourse (due to pain or other reasons) – ask your GP, midwife or health visitor to refer you to our specialist pelvic health physiotherapy team at MKUH.
If you would like further information please refer to our online resources.