Breech Presentation – What are your choices?
Please note, this page is printable by selecting the normal print options on your computer.
This information leaflet aims to support the advice you are given by your midwife and obstetrician if your baby is a breech presentation and will help you to make an informed choice about how your baby may be born.
What is a breech position?
Breech presentation means that your baby is lying bottom first or feet first in the womb (uterus) instead of in the usual head down position. In early pregnancy, it is common for babies to be in a breech position, but as pregnancy continues, a baby usually turns naturally into a head down position, ready to be born. Between 38 and 42 weeks (term) approximately 3 – 4 babies in every 100 are in a breech position. Although some babies may still change position, it is unusual for a baby to turn on its own after this time.
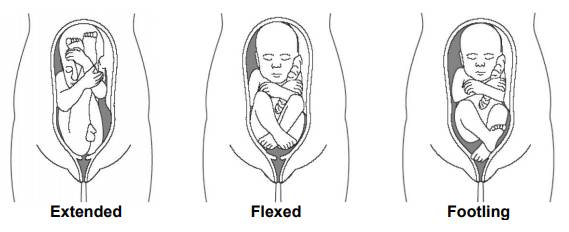
A breech baby may be lying in one of the following positions:
• Extended or Frank breech – The baby is bottom first, with the thighs against the baby’s chest and feet up by the ears. Most breech babies are in this position.
• Flexed breech – the baby is bottom first, with the thighs against the chest and the knees bent.
• Footling breech – one or both feet come first with the bottom in a higher position. This can be common in breech babies who are premature.
Why is my baby breech?
It may just be a matter of chance that your baby has not turned into the head-first position. However, there are certain factors that make it more difficult for your baby to turn during pregnancy and therefore more likely to stay in the breech position. These include:
• if this is your first pregnancy
• if your placenta is in a low-lying position (also known as placenta praevia); see the RCOG patient information Placenta praevia, placenta accreta and vasa praevia
• if you have too much or too little fluid (amniotic fluid) around your baby
• if you are having more than one baby.
Very rarely, breech may be a sign of a problem with the baby. If this is the case, such problems may be picked up during the scan you are offered at around 20 weeks of pregnancy.
What happens if a breech position is suspected?
If your midwife or obstetrician suspects that your baby is in a breech position, an ultrasound scan is used to assess the position and size of the baby. If it is confirmed that your baby is a breech presentation an obstetrician (a obstetrician who specialises in pregnancy and birth) will discuss with you the options for birth.
These choices usually are:
• External cephalic version (using gentle pressure on your abdomen to try and help the baby turn around into a head down position).
• Vaginal Breech birth.
• Planned Caesarean Section.
What is External Cephalic Version or ECV?
ECV improves your chances of a normal birth and involves turning your baby to a head down position in the womb. ECV is usually performed after 36 or 37 weeks of pregnancy. However, it can be performed right up until the early stages of labour. You do not need to make any preparations for your ECV.
An ECV is usually undertaken in the labour ward which takes approximately 10-15 minutes; however, you will be observed for about 1- 2 hours following the procedure. An Obstetrician will perform ECV by placing their hands on the outside of your tummy, feel the position of the baby and then using gentle pressure will encourage your baby to move slowly into the correct position.
Is ECV suitable for everyone with a breech presentation?
An ECV is not appropriate for all women with a breech presentation and should not be performed if:
• It has been recommended that your baby is born by caesarean section for any other reason.
• If you have had a previous caesarean section or uterine surgery.
• If you are expecting twins or more.
• You have had vaginal bleeding during the previous seven days.
• There are concerns about your baby’s heart rate tracing (also known as a CTG).
• If the amount of fluid around your baby is reduced or if your waters have broken before you go into labour.
• Your womb is an unusual shape rather than the usual pear shape.
• There are occasionally other reasons why we may not attempt to turn your baby and we will discuss these with you.
ECV – what happens?
Once a decision has been made to use ECV to turn your baby you will be given a date and time to come into the labour ward. You can eat and drink as normal . The procedure usually involves the following steps:
• Your baby’s heartbeat will be monitored for approximately 20-30 minutes.
• Your baby’s position will be confirmed using an ultrasound scan.
• You may be given a small injection under the skin to relax your womb before the obstetrician attempts to turn your baby.
• You will be asked to either lie on your side or back
• The obstetrician will then use gentle pressure to try and turn your baby.
• After each attempt at turning your baby a check will be made on your baby’s heartbeat.
• Once the procedure is finished an ultrasound will be performed to confirm the position and your baby’s heartbeat will be monitored for another 20-30 minutes and if all is well you will be able to go home.
Is ECV painful?
ECV can be uncomfortable and occasionally painful but your healthcare professional will stop if you are experiencing pain and the procedure will only last for a few minutes. If your healthcare professional is unsuccessful at their first attempt in turning your baby then, with your consent, they may try again on another day.
If your blood type is rhesus D negative, you will be advised to have an anti-D injection after the ECV and to have a blood test. See the NICE patient information Routine antenatal anti-D prophylaxis for women who are rhesus D negative, which is available at: www.nice.org.uk/guidance/ta156/informationforpublic.
If your baby has been turned into a head down position, you may be more comfortable because your baby’s head is now not under your ribcage.
Is ECV safe for me and my baby?
ECV is generally safe. Your baby’s heart rate will be monitored before and after the ECV. Like any medical procedure, complications can sometimes occur. 0.5% of babies (1 in 200) need to be delivered by emergency caesarean section immediately after an ECV. This is usually because of changes in the baby’s heartbeat or more rarely due to the small risk of bleeding from the placenta. For this reason, ECV should always be performed in hospital where there are facilities to perform an emergency caesarean if necessary.
Is ECV successful?
Approximately 50% of breech presentations will turn to a head down position using ECV. Relaxing the muscles of the womb with medication before the ECV improves the chance of success. This
medication will not affect your baby. If it is not possible to turn your baby using ECV your options for birth will be discussed with you before you leave the hospital. A follow up antenatal clinic appointment may also be arranged for you.
What happens after ECV?
If the ECV was successful we will discharge you back to your obstetrician and/or midwife. Occasionally a baby will turn back again to a breech presentation, but this happens to less than 5 in every 100 women who have had a successful ECV. If the procedure is not successful, we will discuss your options for birth and give you time to consider your birth choice. You will then usually have an antenatal clinic appointment where your choice for birth will be discussed and plan for your baby’s birth will be made with you.
At home after ECV
If you experience bleeding, abdominal pain, contractions, reduced movements, if you think your waters have broken or are worried about anything after ECV, you should telephone the labour ward (01908 243478).
Is there anything else I can do to help my baby turn?
There is no scientific evidence that lying down or sitting in a particular position can help your baby to turn. There is some evidence that the use of moxibustion (burning a Chinese herb called
mugwort) at 33–35 weeks of pregnancy may help your baby to turn into the head-first position, possibly by encouraging your baby’s movements. This should be performed under the direction of
a registered healthcare practitioner.
My baby is still in a breech position. What are my choices for birth?
An obstetrician will discuss your options for birth with you at an antenatal clinic appointment, considering your individual circumstances. How you give birth to your baby is your choice. Your
options are usually:
•Vaginal breech birth
• Caesarean section – this is a surgical operation where a cut is made in your abdomen to deliver your baby.
There are benefits and risks associated with both caesarean section and vaginal breech birth, although these are different for both types of birth.
Vaginal breech birth
Many breech babies are born safely vaginally (with their bottoms coming first instead of their head), especially if you have previously had vaginal births without any problems. A hospital birth is
recommended for women whose babies are in a breech position as there is not the expertise to safely manage this type of birth available for home birth. Induction of labour is not usually recommended.
A successful vaginal birth carries the least risks for you, but it does carry a slightly higher risk of serious short-term complications for your baby. However, it does not appear that in most cases
that these have any long-term effects.
If there are no additional risk factors, a vaginal birth may be a suitable option for you. However, it may not be recommended as safe in all circumstances. It can be a more complicated birth, as the
head which is the largest part of the baby is last to be delivered and in some cases, this may be difficult.
A vaginal breech birth will be considered in the following circumstances:
• The baby is not too large or too small .
• The type of breech position is considered safe to attempt vaginal birth.
• Your baby is not lying in a position where its head is hyper-extended (tilted backwards).
• If labour starts naturally.
• There is a obstetrician or midwife available on duty with experience of breech births.
• There are no concerns about where the placenta is sited.
• There are no features about your pregnancy that would make vaginal breech birth unadvisable.
Caesarean Birth
When your baby is in a breech position before birth, the current recommendation of the RCOG and the National Institute for Health and Clinical Excellence (NICE) is that caesarean birth is slightly safer for your baby. Perinatal mortality is 0.5:1000 for Caesarean birth after 39 weeks compared to 2:1000 for vaginal breech birth and 1:1000 for cephalic vaginal birth (RCOG 2017).
Evidence shows that a planned caesarean section is a safe operation, but caesarean birth does have slightly higher risks for the mother, compared with the risk of having a vaginal birth. Serious complications are extremely rare, but a caesarean birth is not without problems.
Common complications of caesarean are infection (1-2 in every 100 women), a higher incidence of blood clots developing in your veins and an above average blood loss (this does not normally cause problems after the operation). Caesarean birth can increase your chances of problems in future pregnancies. These may include placental problems or difficulty with repeat caesarean section surgery. Caesarean birth means a stay in hospital of 1- 2 days, with a longer recovery time. The caesarean birth leaflet will give you further information which your midwife or obstetrician will be able to discuss in more detail with you.
If you choose a caesarean birth we will usually arrange for this to happen after you have reached 39 weeks of pregnancy. Once your caesarean date is arranged we will discuss what to expect and
let you know what is involved. Should you go into labour before the operation, your obstetrician should assess whether it is safe to proceed with the caesarean birth. If the baby is close to being born, it may be safer for you to have a vaginal breech birth.
If you chose a caesarean birth, you will be scanned before the operation to confirm the position of the baby. If your baby has turned and the scan shows that your baby is in a head down position we will not go ahead with the planned caesarean.
What will labour and a breech birth be like?
All labour and birth experiences vary, and a vaginal breech birth need not be more difficult or painful than a birth where the baby is born head down. When your labour has started and you are
having regular contractions you should come into hospital as usual. You can have the same choices of pain relief as with a baby who is head down, except use of the birthing pool. We advise that your baby’s heart rate is monitored continuously in labour to help us assess how well your baby copes with labour.
Midwives and obstetricians will be with you at your baby’s birth and a paediatrician (a children’s obstetrician) and sometimes an anaesthetist will be present when your baby is born. Vaginal breech births can vary slightly in their management, but it is usual for the obstetrician or midwife to avoid touching the baby during birth unless this is necessary. As with all births some require assistance. Provided all is well the obstetrician or midwife avoids intervening unless this is needed.
What happens after my baby is born?
A paediatrician will attend the birth of your baby and afterwards, he or she will have all the usual baby check before you go home. Sometimes baby’s presenting as breech can have problems with their hips. All breech babies need an ultrasound scan to check their hips after their birth. This is usually performed between 4-6 weeks after your baby’s birth. A paediatrician will examine your baby’s hips before you go home and arrange the follow-up ultrasound examination for your baby.
What if my labour is early?
If your baby is born before 37 weeks, the balance of benefits and risks of having a caesarean birth or vaginal birth will be discussed with you. Your choices for birth may be affected by what is
happening and your obstetrician will be able to advise you on the safest option for birth.
What if I’m having twins and one of them is breech?
If you are having twins and the first baby is breech, your obstetrician will usually recommend a caesarean birth. The position of the second twin before labour is less important as the second twin
can change position once the first twin is born, as there is more room for the baby to move. The second twin may either turn to a head down position or remain as a breech presentation. Provided
all is well and there is no need to intervene the second twin may be a vaginal breech birth.
Your choice
There is rarely a straightforward way to advise on what is the best option if you find your baby to be breech towards the end of pregnancy. The most important thing is that you have considered all
the options available and reach a decision that is right for you. You will be offered the opportunity to discuss your individual needs and preferences about how you want to give birth with your midwife and obstetrician and be given sufficient time to think through your options.
Useful contacts:
Community Midwives 01908 996484
Labour Ward 01908 996478/01908 996480
Websites
Midirs Informed Choice Information www.infochoice.org
National Childbirth Trust 0300 330 0700 (option 1) www.nct.org.uk
Royal College of Obstetricians and Gynaecologists www.rcog.org.uk
Obstetric Anaesthetists Association www.oaa-anaes.ac.uk
References:
MIDIRS informed choice leaflet – If your baby is in the breech position, what are your choices? www.midirs.org
NICE (2011) Caesarean section guidance – information for pregnant women, their partners and the public: www.nice.org.uk/Guidance/CG132
RCOG (2017) Management of Breech Presentation (Green-top Guideline No. 20b). www.rcog.org.uk
RCOG (2017) A breech baby at the end of pregnancy – patient information leaflet. www.rcog.org.uk
RCOG (2008) Turning A Breech Baby in the Womb (External Cephalic Version). www.rcog.org.uk
