Last Modified: 4:22pm 07/03/2023
Common pregnancy symptoms or complications
You may experience some symptoms during pregnancy. Most are normal and will not harm you or your baby but if they are severe or you are worried about them, speak to your Midwife or Doctor. You may feel some tiredness, sickness, headaches or other mild aches and pains. Some women experience heartburn, constipation or haemorrhoids. There may also be some swelling of your face, hands or ankles or you may develop varicose veins. Changes in mood and sex drive are also common. Sex is safe unless you are advised otherwise by your healthcare team. Complications in pregnancy require additional visits for extra surveillance of you and your baby’s wellbeing. Many conditions will only improve after giving birth, so it may be necessary to induce your labour or undertake a planned (elective) caesarean section.
Details of previous pregnancies and births are relevant when making decisions about the care you will be offered.
Your healthcare team will need to know important facts such as:
- where you gave birth
- a summary of how your pregnancy went and if you developed any complications
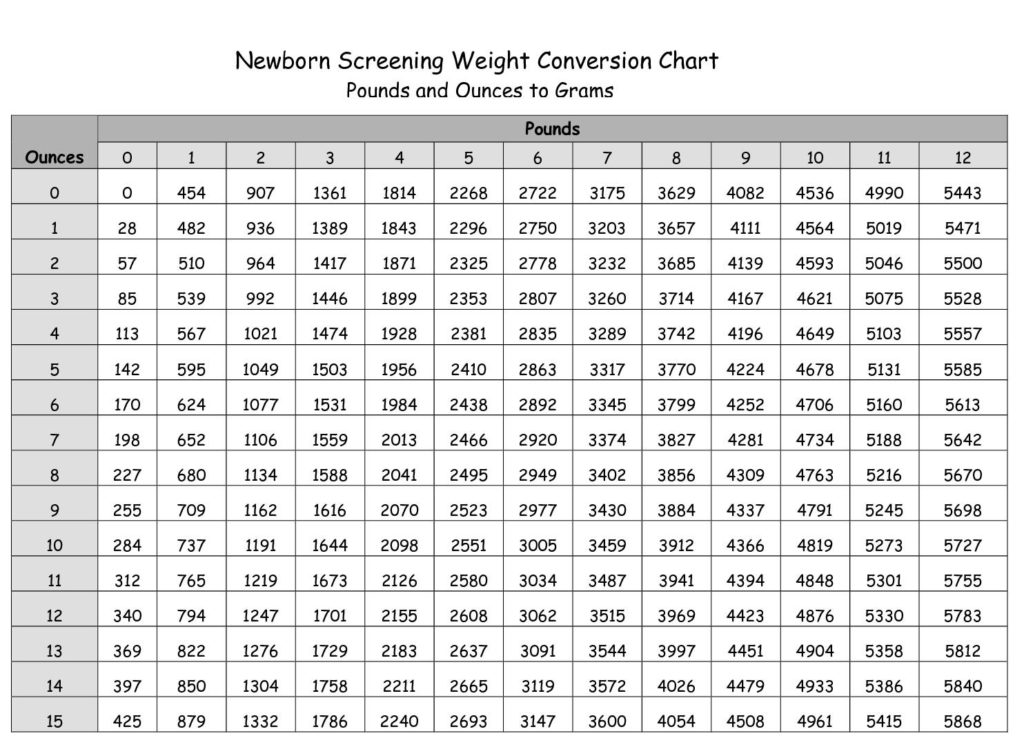
- the weight of your baby and how you and your baby were after the birth.
Para: the term which describes how many babies you already have. Usually early pregnancy losses are also listed after a ‘plus’ sign(+). For example if you had had 2 pregnancies and 1 miscarriage it would say ‘2 + 1’.
Some of the most common problems are outlined below. This information will help you and your healthcare team develop a personalised plan together which will support your choices/preferences. If there is anything else you think may be important, please tell your Midwife or Obstetrician.
► Pregnancy sickness
This is common and for most women symptoms can be managed with changes to their diet and lifestyle. However, it is not uncommon for pregnancy sickness to be severe and have a serious negative impact on the quality of your life and your ability to eat, drink and function normally. If this happens, speak to your GP and request anti-sickness medication. These are safe to take at any stage of pregnancy. It is important to treat pregnancy sickness at an early stage to prevent it from developing into the more serious condition called hyperemesis gravidarum. If you are sick, wait at least 30 minutes before brushing your teeth or using mouthwash. This helps to protect your teeth from tooth decay. For further information on pregnancy sickness and support, click here.
► Abdominal pain
Mild pain in early pregnancy is not uncommon and you may have some discomfort due to your body stretching and changing shape. If you experience severe pain, or pain with vaginal bleeding or need to pass urine more frequently, contact your Midwife or nearest Maternity Unit immediately for advice. Do not wait for your next appointment.
► Vaginal bleeding
This can come from anywhere in the birth canal, including the placenta. Occasionally, there can be an ‘abruption’ where a part of the placenta separates from the uterus which puts the baby at great risk. If the placenta is low lying, tightenings or contractions may also cause bleeding. Any vaginal blood loss should be reported immediately to your Midwife or nearest Maternity Unit. You will be asked to go into hospital for tests, and advised to stay until the bleeding has stopped or the baby is born. If you have rhesus negative blood, you will require an anti-D injection.
► Infections
Your immune system changes when you are pregnant and you are at a higher risk of developing an infection. It is very important that if you are unwell and are experiencing any of the following symptoms, please seek medical advice as treatment may be required:
- high temperature of 38C or higher
- fever and chills
- foul smelling discharge
- painful red blisters/sores around the vagina/bottom or thighs
- pain or frequently passing urine
- abdominal pain
- rash
- diarrhoea and vomiting
- sore throat or respiratory infection.
Avoid unprotected sexual contact if your partner has genital herpes and aviod oral sex from a partner with a cold sore. Wash your hands if you touch the sores.
Wherever possible, keep away from people with an infection.
► Abnormal vaginal discharge
It is normal to have increased vaginal discharge when you are pregnant. It should be clear or white and not smell unpleasant. You need to seek medical advice if the discharge changes colour, smells or you feel sore or itchy.
► High blood pressure and/or pre-eclampsia
Your blood pressure will be checked frequently during pregnancy. A rise in blood pressure can be the first sign of a condition known as pre-eclampsia or pregnancy induced hypertension. Contact your Midwife or nearest Maternity Unit immediately if you get:
- severe headaches
- blurred vision or spots before your eyes
- obvious swelling especially affecting your hands and face
- severe pain below your ribs
- vomiting
as these can be signs that your blood pressure has risen sharply. If there is protein in your urine, you may have pre-eclampsia which in its severe form can cause blood clotting problems and fits. It can be linked to problems for the baby such as growth restriction. Treatment may start with rest, but some women will need medication that lowers high blood pressure. Occasionally this can be the reason a baby needs to be delivered early.
If you had this condition previously, you are more likely to have it again, although it is usually less severe and starts later in pregnancy. It is more likely to happen again if you have a new partner.
► Diabetes
Diabetes is a condition that causes a person’s blood sugar (glucose) level to become too high. It may be pre-existing diabetes htat is present before pregnancy, or some women can develop diabetes during their pregnancy (known as gestational diabetes or GDM). High levels of glucose can cross the placenta and cause the baby to grow large/ If you have pre-existing or gestational diabetes during your pregnancy you will be looked after by a specialist team who will check you and your baby’s health and wellbeing closely. Keeping your blood sugar levels as near to normal as possible can help prevent problems/complications for you and your baby. Gestational diabetes usually disappears after the birth, but can occur in another pregnancy. To reduce your future risks of diabetes:
- have a normal BMI for your height.
- eat healthily
- cut down on sugar, fatty and fried foods
- increase your level of physical activity.
► Thrombosis (clotting in the blood)
Your body naturally has more clotting factors during pregnancy which helps prevent losing too much blood during labour and birth. However, this means that all pregnant women are at a slightly increased risk of developing blood clots during pregnancy and the first weeks after the birth. The risk is higher if you are over 35, have a BMI greater than 30, smoke, or have a family history of thrombosis. Contact your Midwife or nearest Maternity Unit immediately if you have any pain or swelling in your leg, pain in your chest or cough up blood.
► Intrahepatic Cholestasis in Pregnancy (ICP)
Also know as obstetric cholestasis is a liver condition in pregnancy that causes itching on the hands and feet, but it may occur anywhere on your body and is usually worse at night. It affects 1 in 140 women in the UK every year. Having this condition may increase your risk of having a stillbirth so you will receive closer monitoring of you and your baby’s health during your pregnancy. If you have itching, blood tests will be offered to check if you have ICP. Treatment includes medication, regular blood tests and having your baby at or around 37-38 weeks. After the birth, the itching should disappear quite quickly. A blood test to check your liver function will be carried out before you are discharged from hospital after the birth and repeated about 6-12 weeks later.
If you were diagnosed with ICP in a previous pregnancy, you are at an increased risk of developing it again.
► Miscarriages
A miscarriage is when you lose a baby before 24 weeks of pregnancy. If this happens in the first three months of pregnancy, it is known as an early miscarriage. This is very common with 10-20% of pregnancies ending this way. Late miscarriages (after three months but before 24 weeks), are less common (only 1-2% of pregnancies). When a miscarriage happens three or more times in a town, this is called a recurrent miscarriage. Sometimes there is a reason found for recurrent or late miscarriage.
► Premature birth
This means any birth before 37 weeks and this can happen for many reasons. The earlier the baby is born, the more likely that it will have problems and need special or intensive neonatal care. If you are planned to give birth in a birth centre, midwifery unit or at home, you will be advised to transfer your care to a Maternity Unit with a neonatal unit. If labour starts before 34 weeks, most maternity units have a policy of trying to stop labour for at least 1-2 days, whilst offering you steroid injections that help the baby’s lungs to mature. However, once labour is well established it is difficult to stop it. Babies born earlier than 34 weeks may need extra help with breathing, feeding and keeping warm.
The chance of premature birth is increased because of smoking, infection, ruptured membranes, bleeding, or growth restriction with your baby.
Having had a baby prematurely before increases the changes of it happening again.
► Multiple pregnancies
Twins, triplets or other multiple pregnancies need closer monitoring which includes frequent tests and scans, under the care of a specialist healthcare team. You will be advised to have your babies in a consultant led maternity unit that has a neonatal unit. Your healthcare team will discuss your options on how best to deliver your babies. It will depend on how your pregnancy progresses, the position that your babies are lying and whether you have had a previous caesarean section.
► Breech
If your baby is presenting bottom or feet first this is called a breech position. If your baby is breech at 36 weeks, your healthcare team will discuss the following options with you:
- trying to turn your baby (ECV = external cephalic version)
- planned (elective) caesarean section
- or a planned vaginal breech birth.
► Small babies (fetal growth restriction)
If one of your previous babies was growth restricted, there is a chance of it happening again. Arrangements will be made to monitor this baby’s growth more closely, offering ultrasound scans and other tests as necessary.
► Big babies (macrosomia
A baby over 4.5kg is usually considered big – but this also depends on your size and how many weeks pregnant you were when this baby was born. You may be offered a blood test to check for gestational diabetes, which can be linked to having bigger babies.
► Congenital anomaly
These are also known as birth defects or deformities. Some congenital anomalies are detected during pregnancy, at birth or as the baby grows older.
► Placenta praevia
This describes the position of the placenta if it lies low in the womb. If you had this confirmed in the last months of any previous pregnancy, you are at an increased risk of this happening again.
► Placenta acreta
This happens when the placenta embeds itself too deeply in the wall of the womb. This is more common with placenta praevia.
► Bleeding after birth
Postpartum haemorrhage (PPH) means a significant loss of blood after birth (usually 500mls or more). Often this happens when the womb does not contract strongly and quickly enough. There is an increased risk of it happening again in any future pregnancies, so you will be advised to have a review with an Obstetrician during pregnancy to discuss options for your place of birth.
► Postnatal wellbeing
The postnatal perios lasts up to 6 weeks after the birth and it is during this time your body recovers. However, for some women problems can occur e.g. slow perineal or wound healing, concerns with passing urine, wind and/or stools. Some women may experience mental health problems.
► Group B Streptococcus (GBS)
GBS is a common bacterium carried by some women and rarely causes symptoms or harm. It can be detected by testing a urine sample or a vaginal or rectal swab. In some pregnancies, it can be passed on to the baby around the time of birth, which can lead to serious illness in the baby. The national recommendation is to offer antibiotics to women as soon as labour starts if:
- GBS has been detected during the current pregnancy
- you have previously had a baby who developed a GBS infection
- you have a high temperature (38C or above) in labour
- you go into labour prematurely.
If you’ve previously had a baby who was diagnosed with a GBS infection after birth, you will be offered intravenous (drip) antibiotics when labour begins. The aim of offering you antibiotics in labour is to reduce the risk of a GBS infection for this baby.
