Vaginal Hysterectomy for Uterine Prolapse and Vaginal Repair
Please note, this page is printable by selecting the normal print options on your computer.
About this leaflet
We advise you to take your time to read this leaflet, any questions you have please write them down on the sheet provided (towards the back) and we can discuss them with you at our next meeting. It is your right to know about the operations being proposed, why they are being proposed, what alternatives there are and what the risks are. These should be covered in this leaflet. This leaflet firstly describes what a Vaginal Hysterectomy is, it then goes on to describe what alternatives are available within our trust, the risks involved in surgery and finally what operation we can offer.
What is Uterine Prolapse
• The uterus is the medical name for the womb. It includes the neck of the womb (cervix) from where the smear test is taken.
• After the menopause (the change) periods stop and the womb is no longer needed for babies. As hormone levels fall at this time, the womb usually gets a bit smaller.
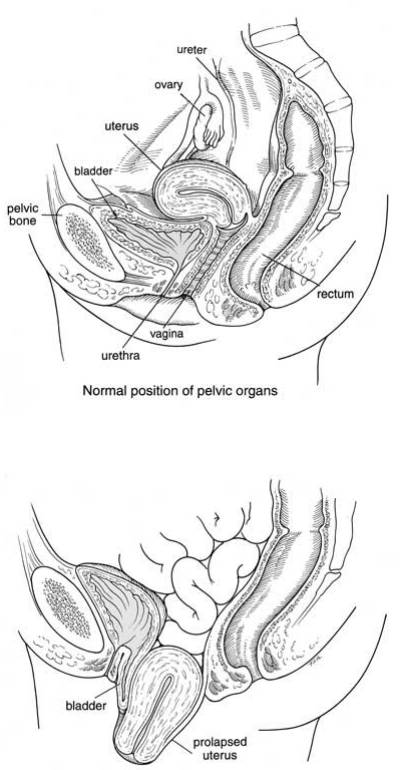
• The womb normally sits in the pelvis which is the place between the hip bones at the bottom of the abdomen (tummy). The pelvic bones form a strong circle and have a sheet of muscles forming a hammock between them – these muscles are the pelvic floor muscles.
• The pelvic floor muscles support the womb, the top of the vagina (front passage), the bladder and the rectum (back passage). If this muscle sheet is weak, the organs it supports can sag down with gravity. Having babies and getting older may weaken the pelvic floor muscles.
• This sagging forms bulges into the vagina because the walls of the vagina are stretchy. This sagging is called Prolapse.
• When the womb is sagging it is called Uterine Prolapse. Sometimes the womb sags so much that the neck of the womb pokes out of the vaginal opening.
• Uterine prolapse can cause you to have a lump in the vagina that you can see or feel. The lump is often smaller first thing in the morning but gets bigger during the day when you are on your feet. The lump can be uncomfortable and it may get in the way of having sex or putting in tampons. If the lump pokes out, it can rub on your underwear and get sore and sometimes gets in the way of the bladder emptying properly
Alternatives to surgery
• Do nothing – if the prolapse (bulge) is not distressing then treatment is not necessarily needed. If, however, the prolapse permanently protrudes through the opening to the vagina and is exposed to the air, it may become dried out and eventually ulcerate. Even if it is not causing symptoms in this situation it is probably best to push it back with a ring pessary (see below) or have an operation to repair it.
• Pelvic floor exercises (PFE) – The pelvic floor muscle runs from the coccyx at the back to the pubic bone at the front and off to the sides. This muscle supports your pelvic organs (uterus, vagina, bladder and rectum). Any muscle in the body needs exercise to keep it strong so that it functions properly. This is more important if that muscle has been damaged. PFE can strengthen the pelvic floor and therefore give more support to the pelvic organs. These exercises may not get rid of the prolapse but they make you more comfortable. PFE are best taught by an expert who is usually a Physiotherapist. These exercises have no risk and even if surgery is required at a later date, they will help your overall chance of being more comfortable.
Types of Pessary
• Ring pessary – this is a soft plastic ring or device which is inserted into the vagina and pushes the prolapse back up. This usually gets rid of the dragging sensation and can improve urinary and bowel symptoms. It needs to be changed every 6-9 months and can be very popular; we can show you an example in clinic. Other pessaries may be used if the Ring pessary is not suitable. Some couples feel that the pessary gets in the way during sexual intercourse, but many couples are not bothered by it.
• Shelf Pessary or Gellhorn – If you are not sexually active this is a stronger pessary which can be inserted into the vagina and needs changing every 4-6 months.
Operations available for Uterine Prolapse
There are several operations which can be performed for Uterine Prolapse. Often your doctor will advise you regarding one of these operations after considering your symptoms, whether you want more children, any medical problems you may have and any treatments you may have tried before in the past. It is important that you have time in clinic to talk about this with your doctor. The most common operation for Uterine Prolapse is a Vaginal Hysterectomy. It involves taking out the womb through the vagina so there are no cuts on your abdomen.
As the womb is removed, this operation is not suitable for women who want more children. If you have not gone through the Menopause (change) and might want more children you must discuss this with your doctor. It may be better for you to do nothing or use a Pessary until you have had your family. The prolapse lump may get worse during pregnancy and not improve once the baby has been born. Having a prolapse does not usually stop you from having a normal delivery. Some types of Pessary can be used in pregnancy.
It is sometimes possible to do an operation for uterine prolapse but leave the womb behind. These operations use strong stitches or artificial mesh (like netting) to hold the womb up in its normal position. Your doctor can discuss these with you. They may want you to see another doctor at a different hospital where they have experience of these operations and can give you advice about them.
If you have a hysterectomy:
• You will not be able to get pregnant
• You will have no more monthly periods
• You will not need to use contraception
• It may be part of a continuing problem or it may mean the end of the health problem
A hysterectomy does not:
• Cause premature aging
• Mean becoming less of a women or losing your sex drive
• Leave a gap inside- the bowel fills up the space
General Risks of Surgery
• Anaesthetic risk – This is very small unless you have specific medical problems. This will be discussed with you.
• Haemorrhage – There is a risk of bleeding with any operation. This may occur during the operation ( 1 in 50 ) or after the operation ( I in 75 ).
• The risk from blood loss is reduced by knowing your blood group beforehand and then having blood available to give you if needed. It is rare that we have to transfuse patients after their operation. Please let your doctor know if you are taking an anti-clotting drug such as warfarin or aspirin.
• Infection – There is a risk of infection at any of the wound sites. A significant infection is rare. The risk of infection is reduced by our policy of routinely giving antibiotics with major surgery. The infection may occur inside the abdomen or in the pelvis. ( 1 in 500 women)
• Deep Vein Thrombosis (DVT) – This is a clot in the deep veins of the leg. The overall risk is at most 4-5% although the majority of these are without symptoms. Occasionally this clot can migrate to the lungs which can be very serious and in rare circumstances it can be fatal (less than 1% of those who get a clot). DVT can occur more often with major operations around the pelvis and the risk increases with obesity, gross varicose veins, infection, immobility and other medical problems. The risk is significantly reduced by using special stockings and injections to thin the blood (heparin).
Specific risks of a Vaginal Hysterectomy
Some risks are specific to operations for prolapse and some risks are special to just a vaginal hysterectomy. You should have the opportunity to discuss these with your doctor.
• Getting another prolapse – Unfortunately having a vaginal hysterectomy does not always stop you from getting a further prolapse. Although the womb has been removed, the vaginal walls or the top of the vagina (the vault) can sag with time. About 1 in 3 women who have an operation for prolapse get another prolapse during their lifetime. This second prolapse may not cause them bother.
Keeping your weight normal for your height, avoiding unnecessary heavy lifting, and not straining on the toilet, will help prevent a further prolapse although even adhering to this sometimes does not prevent a further prolapse.
• A change in the way your bladder works – Having a prolapse sometimes causes some kinking to the exit of your bladder. This can be enough to stop urine leaks on coughing, laughing or sneezing caused by a weak bladder. By removing the prolapse this kink gets straightened out and the leaks are no longer stopped. If your doctor thinks this might happen to you, they may suggest having some bladder tests before the operation so that you know what the risks are.
After a vaginal hysterectomy, the bladder becomes irritable or overactive in up to 15% of women. This means that for every 100 women who have a vaginal hysterectomy, 15 get an irritable or overactive bladder that they didn’t have before. This gives symptoms like needing to rush to the toilet or needing to pass urine more often. Sometimes an overactive bladder can make you leak because you can’t get to the toilet in time.
• A change in the way your bowel works – Having some constipation after an operation is very common and this usually settles quickly. Women rarely find their bowels have changed after a vaginal hysterectomy.
• Needing to make a cut in your abdomen (tummy) – occasionally an incision is required in the abdomen to remove the womb. This may be because there is heavy bleeding making it difficult to see or because the womb is much bigger than expected or because there is scar tissue from a past operation sticking to the womb. If the incision is needed it is usually a bikini line cut. A hysterectomy via the abdomen (abdominal hysterectomy) is usually more painful than a vaginal hysterectomy so you may need extra painkillers and a bit longer in hospital. Your doctor will explain why it was needed so you know what happened in the operating theatre.
• Damage to the bladder or bowel – During the operation, cuts and stitches are made very near the bladder, ureter (tube taking urine from kidney to the bladder), and bowel, and occasionally the surgeon may make a hole in the bladder ( one in 150 women)or bowel ( one in 2500) by accident. It is usually possible to repair the hole straight away but it may affect your recovery. Your doctor will explain what happened and what, if anything, needs to be done about it.
• Painful sexual intercourse – Once the wound at the top of the vagina has healed, there is nothing to stop you from having sex. The healing usually takes about 6 weeks. Some women find sex is uncomfortable at first but it gets better with time and sometimes improves using a bit of extra lubrication (YES Cream or Gel, Sylk, Replens or alternative vaginal lubricant). Sometimes sex continues to be painful after the healing has finished but this is rare especially if only a vaginal hysterectomy has been performed.
• Change in sensation with intercourse – Sometimes the sensation during intercourse may be less and occasionally the orgasm may be less intense.
What happens during a Vaginal Hysterectomy?
• The operation can be done with a general anaesthetic so you are asleep or using a spinal anaesthetic so you are awake but unable to feel any pain from the waist down.
• Your legs are placed in stirrups (to elevate them) and the vagina and surrounding skin cleaned with antiseptic solution.
• Often some local anaesthetic will be injected into the vagina even if you are asleep as it can help to make the operation easier and reduce bleeding.
• A cut is made around the neck of the womb (cervix). Alongside the womb are strong ligaments (which help to hold the womb up) and the blood vessels to and from the womb. These are cut and tied off with dissolvable stitches.
• The womb is taken out and sent to the laboratory so that they can look at it under a microscope and check it is a normal womb.
• The hole at the top of the vagina is stitched closed with dissolvable stitches. Once it has healed, the vagina will have a smooth top.
• Usually a catheter tube is passed along the urethra (water pipe) to drain the bladder. Once any swelling around the bladder has gone down, this will be removed.
• Sometimes a long bandage called a ‘pack’ will be put in the vagina to press on the wound and soak up any spilled blood. This is removed the next day.
• You usually stay in hospital for up to five days. Other operations performed at the same time.
Your doctor may suggest that a Vaginal Hysterectomy is all that is required to help your prolapse. However, sometimes extra operations are done at the same time as a Vaginal Hysterectomy and your doctor may advise you regarding these. You should check that you know exactly what will happen to you in the operating theatre and why any extra operations are or are not being suggested.
• Removal of the ovaries and fallopian tubes – The ovaries are usually left behind during a Vaginal Hysterectomy. This is because they are quite high up in the pelvis and can be difficult to reach when taking the womb out vaginally. The ovaries are not involved in prolapse and don’t need to be taken out to treat a prolapse. If there is a special reason why you need your ovaries taking out, you should discuss this with your doctor. They may suggest leaving them behind or taking them out through your abdomen (tummy), perhaps with keyhole surgery. The fallopian tubes can be taken out in order to reduce the risk of endometrial and ovarian cancer.
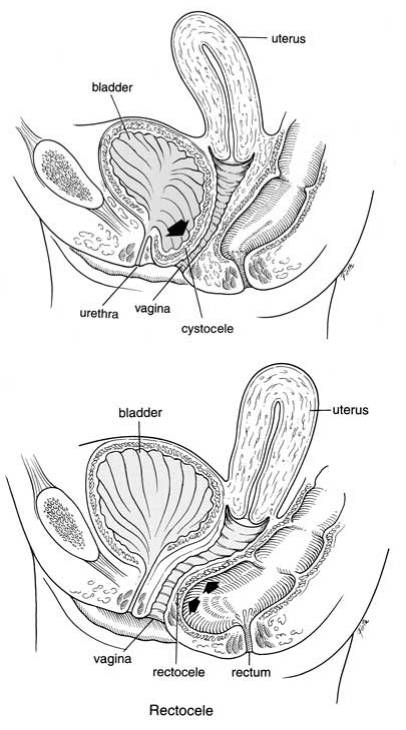
• Vaginal repairs – Often the vaginal walls sag when the womb sags. Sometimes the front (anterior, called cystocele) or back (posterior, called rectocele) walls of the vagina sag so much that your doctor may suggest repairing them at the same time as your hysterectomy. This shouldn’t make your stay in hospital any longer and the recovery at home is much the same. However, some things are different including the risks of the operation. For example, painful intercourse (sex) is more likely if a repair is done, although it is still uncommon. You should, therefore discuss this with your doctor. They may have an extra information leaflet for you about vaginal wall repairs.
Sacrospinous fixation (SSF) – If your doctor is worried that the top of the vagina will sag down as soon as the womb is out, they may suggest a SSF. This involves holding the top of the vagina up by stitching it to a strong ligament in the pelvis. It is done through a cut on the back wall of the vagina so it might be combined with a back wall repair. There is another information leaflet about the SSF operation which you should be given if you are thinking about having it done.
After the operation – in hospital
On return from the operating theatre you will have a fine tube (drip) in one of your arm veins with fluid running through to stop you getting dehydrated. You may have a bandage in the vagina, called a ‘pack’ and a sanitary pad in place. This is to apply pressure to the wound to stop it oozing. You may have a tube (catheter) draining the bladder overnight. The catheter may give you the sensation as though you need to pass urine but this is not the case. Usually the drip, pack and catheter come out the morning after surgery or sometimes later the same day. This is not generally painful. The day after the operation you will be encouraged to get out of bed and take short walks around the ward. This improves general wellbeing and reduces the risk of clots on the legs.
It is important that the amount of urine is measured the first couple of times you pass urine after the removal of the catheter. An ultrasound scan for your bladder may be done on the ward to make sure that you are emptying your bladder properly. If you are leaving a significant amount of urine in your bladder, you may have to have the catheter re-inserted into your bladder for a couple of days more. You may be given injections to keep your blood thin and reduce the risk of blood clots normally once a day until you go home or longer in some cases. The wound is not normally very painful but sometimes you may require tablets or injections for pain relief.
There will be slight vaginal bleeding like the end of a period after the operation. This may last for a few weeks. Your vaginal loss should change to a creamy discharge over the next 2-3 weeks. ( if you have any new pain, fresh bleeding or bad smelling discharge after you go home, you should contact your GP). The nurses will advise you about sick notes, certificates etc. You are usually in
hospital for 2-4 days.
Recovery after the operation – at home
Mobilization is very important; using your leg muscles will reduce the risk of clots in the back of the legs (DVT), which can be very dangerous. You are likely to feel tired and may need to rest in the daytime from time to time for a month or more, this will gradually improve. It is important to avoid stretching the repair particularly in the first weeks after surgery. Therefore, avoid constipation and heavy lifting. The deep stitches dissolve during the first three months and the body will gradually lay down strong scar tissue over a few months.
Avoiding constipation
• Drink plenty of water / juice
• Eat fruit and green vegetables especially broccoli
• Plenty of roughage e.g. bran / oats
Do not use tampons for 6 weeks. There are stitches in the skin wound in the vagina. Any of the stitches under the skin will melt away by themselves. The surface knots of the stitches may appear on your underwear or pads after about two weeks, this is quite normal. There may be little bleeding again after about two weeks when the surface knots fall off, this is nothing to worry about. At six weeks gradually build up your level of activity. After 3 months, you should be able to return completely to your usual level of activity.
You should be able to return to a light job after about six weeks, a busy job in 12 weeks. Avoid all unnecessary heavy lifting. You can drive as soon as you can make an emergency stop without discomfort, generally after three weeks, but you must check this with your insurance company, as some of them insist that you should wait for six weeks.
Sex after hysterectomy
There may be a change in sexual response after hysterectomy. For many women it is improved because there is no longer discomfort or the risk of pregnancy. You can start sexual relations whenever you feel comfortable enough after six weeks, so long as you have no blood loss. You will need to be gentle and may wish to use lubrication (KY jelly) as some of the internal knots could cause your partner discomfort. You may, otherwise, wish to defer sexual intercourse until all the stitches have dissolved, typically 3-4 months.
Unless a prolapse has been repaired, the vagina should not be smaller, but it take a while for the scarring at the top to become supple. Intercourse will help this. Because the womb has been removed, contractions that may have been felt during the orgasm will no longer occur.
Emotional effects
Some women may experience an emotional reaction after a hysterectomy, although removing the disabling symptoms are normally welcomed. If these problems persist you should discuss them with your GP.
Follow up
After the operation is usually six weeks to six months. This maybe at the hospital (doctor or nurse), with your GP or by telephone. Sometimes follow up is not required. You don’t need to have future smear test as the cervix will be removed during vaginal hysterectomy.
More information about Uterine Prolapse
If you would like to know more about uterine prolapse and the treatments available for it, you may try the following sources of information.
• Ask your GP.
• Ask the Doctor or Nurse at the hospital.
• Look at a website such as
NHS choices at www.nhs.uk/conditions/Hysterectomy
Or
www.nhs.uk/conditions/prolapse-of-the-uterus
Or
Patient UK at www.patient.co.uk
Or
*The Hysterectomy Association at www.hysterectomyassociation.org.uk
Or
http://pogp.csp.org.uk/publications/pelvic-organ-prolapsephysiotherapy-guide-women
Or
https://bsug.org.uk/
Reference: The information in this leaflet is based on British Society of Urogynaecologist information leaflet: vaginal hysterectomy for uterine prolapse
