Urinary Incontinence
Please note, this page is printable by selecting the normal print options on your computer.
What is it?
Urinary incontinence is a common problem, which can cause embarrassment and distress, and is often easily treatable. It can occur at any age, but incidence increases with age. It is thought that there are 3 million people in the UK who are incontinent. Sufferers of urinary incontinence tend to leak urine when they are not wishing to pass urine. This can be anything from a small dribble, periodically to large floods.
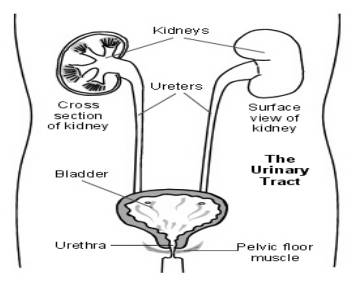
Urine is made by the kidneys all the time and passes down to the bladder through the ureters (tubes), where it is stored. The volume of urine produced is dependant on how much you drink. The bladder is like a balloon and expands, as it fills with urine. The outlet for urine (urethra) is normally kept closed, helped by the pelvic floor muscles beneath the bladder. These then both relax and the bladder muscle contracts, when the bladder gets full and you go to the toilet to pass urine. Nerve messages which pass between the brain, bladder and pelvic floor muscles tell you when your bladder is full and when the muscles need to contract and relax.
Types
Stress Incontinence – Occurs because the pelvic floor muscles are weak and when the pressure within the bladder becomes too great for the outlet to withstand. Leakage often occurs when you cough, laugh or exercise (activities which increase intraabdominal pressure). This is most commonly related to child birth, which causes the pelvic floor to weaken.
Urge Incontinence – This is when you get an urgent desire to pass urine and is possibly due to an overactive bladder muscle. Urine often leaks before you have a chance to get to the toilet.
Help and Treatment
Lifestyle Changes:
Reducing the amount of caffeine, carbonated drinks and alcohol you drink, can be beneficial, because caffeine has a diuretic effect (you will pass urine more often) and it also stimulates the bladder directly. You should modify your fluid intake, so that it is not too much or too little, this should ideally be 2 litres (6 – 8 cups) a day. Reducing intake 2 hours prior to going to bed can also help. Losing weight may help with the problem.
Bladder Diary:
This will be useful for when you are assessed. It gives doctors a clear picture of what your bladder habits are. Make a note of the times you pass urine, and the amount (volume) that you pass each time. Also make a note of the times you leak urine (are incontinent) and what your fluid intake is like. Try and complete the diary for a minimum of 3 days to cover variations in activities and work/leisure days.
Bladder Training:
The aim is to slowly stretch the bladder so that it can hold larger and larger volumes of urine. In time, the bladder muscle should become less overactive and you become more in control of your bladder. Go to the toilet only when you need to. If you go to the toilet too often, the bladder becomes used to holding less urine. Bladder training can be difficult, but becomes easier with time.
Pelvic Floor Exercises:
The pelvic floor is a hammock-like group of muscles at the base of the pelvis. They help to support the organs in the abdomen and pelvis, and control the bladder and bowel. Strengthening them will help with leakage. Sit in an upright position. Imagine that you are trying to stop yourself passing urine and ‘wind’ by squeezing and lifting the openings of the bladder and bowels. ‘Squeeze and lift’ and try to hold for a few seconds. (Breathe normally – don’t hold your breath!) Rest for a moment, and then repeat another 4 times if you can. Now try squeezing the pelvic floor muscles quickly 5 times. This helps your muscles react quickly when you cough or sneeze to prevent leakage of urine.
Aim to do 5 slow and 5 fast squeezes up to 4 times a day, gradually building up the repetitions to a maximum of 10 times, held for 10 seconds each. Don’t try to stop and start your urine flow midstream. This can interfere with normal bladder function. 6 out of 10 cases of stress incontinence can be cured or much improved by these exercises. It works best if combined with advice and support from a physiotherapist, continence advisor, nurse, or doctor.
Medication and surgical management
Medication including anticholingeric and B3 adrenonreceptors (Mirobegron) may help for overactive bladder. They work by blocking certain nerve impulses to the bladder which ‘relaxes’ the
bladder muscle and so increases the bladder capacity. It is usual to start with a course of 4-6 weeks prior to see any benefit, progressing to 6 months or more if symptoms improve. Results tend to vary from person to person. The side effects including dry mouth, constipation and dry eyes are seen more with anticholinergics and are more severe at the beginning. Usually after a few weeks the body adopts and the side effects are less bothersome.
For stress incontinence the main help after pelvic floor exercises is a surgical approach. The available surgical approaches at this Trust are injection of bulking agents (Bulkamid) or a colposuspension (tightening the bladder neck with sutures through an abdominal incision). These procedures prevent leakage of urine on activities which increase pressure inside the abdomen (such as coughing, sneezing or running). If you don’t respond to physiotherapy and pelvic floor exercises, medication, have mixed incontinence and suffer from a combination of prolapse and
incontinence or prior to any surgical management you need to have further investigation including urodynamic study (UDS) (Please refer to UDS leaflet).
Further Help and Information
Continence Foundation
307 Hatton Square
16 Baldwin Gardens
London, EC1N 7RG Tel (Helpline): 0845 345 0165
Web: http://www.continence-foundation.org.uk/
Urogynaecology Nurse Specialist 01908 997119
Consultant secretary 01908 997318
For further advice on incontinence the Milton Keynes Primary Care Trust has a Continence Advisor who can be contacted via your GP surgery. Please bring your bladder diary with you if attending a clinic and be prepared for urine sample and an internal examination.
