Suspected Pulmonary Embolism in Pregnant Women
Please note, this page is printable by selecting the normal print options on your computer.
What is Pulmonary Embolism (P.E)?
Blood flows through your body in veins and arteries. If a blood clot forms in a deep vein in the leg it is called a Deep Vein Thrombosis (DVT). A Pulmonary Embolism (PE) is when part of this clot becomes loose. Travels through the veins and suddenly blocks an artery in the lungs, this is why you may feel breathless.
What symptoms might I have with a DVT or a PE?
A DVT causes swelling, pain and skin reddening in the leg, most commonly below the knee in the calf.
A PE can cause:
• sudden unexplained difficulty in breathing
• tightness in the chest or chest pain
• coughing up blood
• an increased heart rate or palpitations.
How common is a PE and why is it important to diagnose?
• Women have a five times increased risk of developing a PE both during pregnancy and for up to six weeks after delivery. Although rare, it can be life-threatening and is one of the most common causes of maternal death in pregnancy.
• If your doctor is concerned that you might have a PE, it is very important that you have tests to confirm this diagnosis. It is important to know about a PE before you go into labour, for future
contraceptive choices and in planning further pregnancies.
• Just because you have some or all of the symptoms listed above does not mean you have a PE. A normal pregnancy or other problems such as a chest infection or a collapsed lung can also cause similar symptoms.
What tests will I need to make the diagnosis?
If there is concern you might have a PE, the doctors looking after you will take advice from a Consultant Radiologist about which tests you should have and in which order. They could include:
• Chest x-ray
• Doppler ultrasound scan of the legs
• Lung perfusion scan (VQ scan)
• CT pulmonary angiogram (CTPA).
It is usual to have more than one test to reach a diagnosis. Some of these tests will expose you and your baby to radiation.
What is radiation?
Radiation is a form of energy which we are exposed to on a daily basis in the form of background radiation. For example, when we go on an aeroplane we are exposed to a higher amount of radiation than when we walk around on the ground. It can be helpful to understand how much radiation we are exposed to during some of tests listed below by calculating the equivalent background radiation dose, eg, chest x-ray is the equivalent of three days background radiation or a four-hour flight. The radiation doses you will be exposed to will be kept as low as possible. This will reduce the amount of radiation that reaches your baby.
What happens when I have tests for PE?
• Chest x-ray
This is a low dose test for you and your baby to check that your symptoms are not due to a collapsed lung, broken rib or chest infection.
• Doppler scan of legs
This is the same type of scan used to monitor your baby during pregnancy. It looks for blood clots in the leg (a DVT). If this scan detects a DVT, no further tests are usually necessary. There is no
radiation involved.
• Lung perfusion scan
You will have injection of a radioactive substance into a vein in your arm and be asked to lie on a table for approximately 30 minutes. This test checks for clots in the blood vessels in the lungs but
cannot assess for any other causes of your symptoms. It is normally not suitable for you if you have an abnormal chest x-ray, asthma, or any other lung disease.
• CT pulmonary angiogram
This is a specialised x-ray of the chest. You will be asked to lie on the scanner table and will have an injection of dye into a vein in your arm at the same time as a CT scan of your chest is being
performed. It normally takes about 10 minutes. The dye contains a substance called iodine, which helps to show up blood clots in the arteries in the lungs. This test can diagnose other abnormalities, not just pulmonary emboli. It cannot be done if you have an iodine allergy or have had an allergic reaction to a previous x-ray contrast.
If you are currently pregnant:
Perfusion scan
The radioactive substance in the injection is removed from the body in the urine. For 24 hours after this test it is important to drink extra fluids and pass urine frequently. As your bladder, which contains the radioactive urine, is next to the baby in the pelvis, the radiation exposure to the baby will reduce by drinking more fluids and passing urine more frequently.
CT pulmonary angiogram
All new babies routinely have a blood test called a Newborn Bloodspot Screening Test 5-8 days after birth, which checks the baby’s thyroid function. If the result is abnormal, a copy of the blood
test report will be forwarded to your GP and a consultant paediatrician. There is a very small risk that the iodine in the x-ray contrast injection could temporarily affect the baby’s thyroid function.
If your baby has an abnormal thyroid function test result, it is important to tell the doctors looking after your baby that you have had this x-ray contrast injection when you were pregnant. After this scan your GP will receive a letter telling him/her that you have had this injection and a copy will also be sent to you to keep.
If you have delivered and are breastfeeding:
The nuclear medicine department performing the scan will provide you with information regarding breastfeeding.
Holding your baby
The nuclear medicine department performing the scan will provide you with information regarding whether you need to restrict prolonged close contact with your baby for a period after the scan.
CT Pulmonary Angiogram:
Breastfeeding
• The current advice from the manufacturers of the x-ray contrast is that you may continue to breastfeed as normal because only very small amounts of contrast are excreted into the breast milk and it is poorly absorbed by the baby’s gut
• Previously, the manufacturer’s advice was to express a feed before the scan and store it. Following the scan, express as much milk as possible and then discard it. The baby should then be fed the milk that has been previously expressed. Breastfeeding should then continue as normal. Some mothers prefer to do this even though it is no longer recommended by the manufacturer. There are no restrictions on holding your baby.
Are these tests safe for me and my baby?
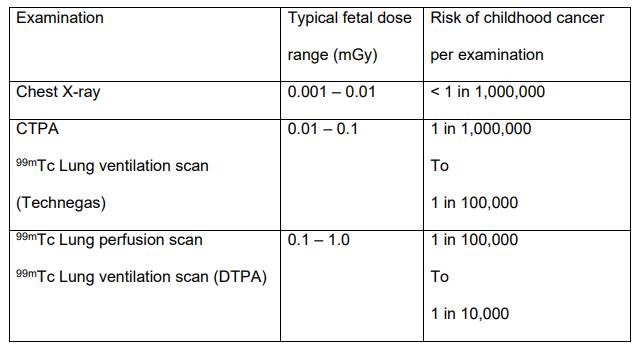
All the tests that involve radiation carry a small risk to you and your baby. This risk has been considered against the benefit to you of having the test and the benefit has been considered to outweigh the risk. Typical radiation doses and risks for the tests described are:
The radiology staff will ensure you are happy to proceed with the tests and will answer any further questions regarding the radiation dose to you and your baby. Please be assured staff will protect your baby as much as possible throughout the examination, by using lead shielding where appropriate and keeping radiation doses as low as reasonably practicable.
Other risks
Rarely the contrast injection can cause an allergic reaction or affect the kidney function. The radiation doses from both examinations are small. The only known effect to the exposed individual at these low doses is a very slight increase in the chance of cancer occurring, many years or even decades after radiation exposure.
Conclusion
The small risks of these scans have to be weighed up against the risk to both mother and baby of an undiagnosed and untreated pulmonary embolus. This is a potentially life threatening condition – the risk of dying from an untreated PE is 15-30%. If there is concern that you might have a PE, further tests are essential to confirm the diagnosis. Radiation doses are kept as low as possible for both you and the baby and are well below the level considered to be harmful for your baby.
If you have any other concerns, please do not hesitate to ask the doctors looking after you who is overseeing your investigations who can provide with further details regarding the result. If the scan shows you do not have a PE further investigations and treatment may be required, if not you will be discharged back to the care of your GP. A letter will be posted to them with a copy for yourself. If the scan shows that you do have a P.E. treatment will be commenced straight away. A Pulmonary Embolism can be a life-threatening condition if not treated. It is vital that you are reassessed by a Doctor if your condition changes at any time for example if you become more breathless.
You will have regular appointments with the Nurse Specialist who will offer you all the information, support, and advice you will require. An out-patient appointment will be made for you to see the Consultant who is a specialist in this condition to discuss your care and to answer any questions you may have.
When to seek emergency help
If at any time you become more breathless, have increasing chest pain, cough or cough up blood or any other concerns please go to your local Accident and Emergency Department or GP.
References
• Suspected PE in Pregnant women, Colchester University Hospital, August 2014
• Protection of pregnant patients during diagnostic medical exposures to ionising radiation. Health Protection Agency RCE-9, 2009.
• https://www.gov.uk/government/publications/medical-radiation-patient-doses/patient-doseinformation-guidance
• https://www.gov.uk/government/publications/medical-and-dental-x-rays-frequency-andcollective-doses-in-the-uk
• Having a V/Q scan or CTPA scan of your lungs whilst Pregnant Patient Information leaflet, University of Leicester
