Staying comfortable during labour
Please note, this page is printable by selecting the normal print options on your computer.
This leaflet outlines the options available to support you during your labour and birth. Many of the options you and your birth partner can do at home, as well as in hospital.
Preparing for labour
You can prepare for birth by attending antenatal classes, talking to your Midwife, and researching information on how to manage your labour. You can write down your ideas in your birth plan and
this can be included in your personalised care plan.
The three stages of labour
The first stage – this includes an early or latent phase, as well as an established phase. Early labour can vary in duration from person to person. During this phase the neck of the womb begins to shorten and soften (known as effacement) and will start to open (dilate) up to 4cm. Contractions are often irregular, short lasting and not as strong as the established phase of labour but they can still be quite intense. During established labour the cervix opens from 4cm to 10cm (fully dilated), and you experience regular and strong contractions.
The second stage – this is when your cervix has opened fully until the birth of your baby.
The third stage – from the birth of your baby until the placenta is birthed, it may last up to an hour, and you may feel mild contractions during this time.
Evidence shows that labour can be a better experience when you:
• Feel relaxed, knowing what is happening within your body
• Keep active and try to get into comfortable positions
• Use breathing techniques
• Have emotional support and encouragement from a birth partner you trust
• Know what is available to help you through your experience
• Feel safe within your birthing environment
• Personalise the environment: you may want to play your own music, use your own pillow, or use electronic tea lights.
What is available at MKUH?
Massage
Can be invaluable during a contraction and releases endorphins (your natural pain-relieving hormones). Your chosen birth partner or midwife can help with this.
Breathing and relaxation techniques
Breathe slowly and rhythmically throughout the contraction and try to relax and stay focused. Your midwife will be able to coach you through different breathing techniques.
Changing positions
Remaining upright and mobile using equipment for support such as beanbags, cub cushions, birthing balls, peanut ball and birthing mat. The hospital bed can be adjusted to support various positions.
Aromatherapy oils
These can be used with other forms of pain relief and are helpful in reducing stress, anxiety, sickness and helping with pain while refreshing or revitalising you. The oils can be used through massage, inhalation or in the birthing pool.
Water
Many find that using a birthing pool or shower can help ease pain and aid relaxation, which encourages the release of endorphins. There are two birthing pools on our labour ward with the option of dimmed lights and a relaxed atmosphere.
Transcutaneous Electrical Nerve Stimulation (TENS)
This is a machine which can help to reduce the pain by blocking the nerve signals to the brain and releasing your natural endorphins. It is controlled by you and is most effective when started in the early stage of labour. These machines are not available at the hospital but can be hired.
Hypnobirthing
If you wish to have a hypno-birth and have attended antenatal preparation in hypnobirthing, the midwives will support you through your labour and birth. All the above can support you at different stages of your labour and have no side effects to you or your baby.
Medicinal forms of pain relief available
Paracetamol
This can be effective during early labour. It can be taken every 4-6 hours according to instructions, with a maximum of four doses in 24 hours.
Dihydrocodeine
Another medication that can be effective during early labour. It can be taken every 4-6 hours according to the prescription.
Entonox (also known as gas and air)
This is breathed through a mouthpiece (50% oxygen, 50% nitrous oxide). It takes about 15 seconds to take effect and is used throughout a contraction. It can help you to manage and help to
focus your breathing through the contraction, with no effect for baby. A few women may feel a little sick or lightheaded, but once they stop breathing the Entonox, that feeling will pass. Another side effect of Entonox is getting a dry mouth, so you will need to have a drink to hand for after the contraction.
Pethidine
This is a pain-relieving drug given by injection that takes approximately 15 minutes to have an effect. It can make the contractions more manageable and help you to relax. It can be given, if required, every 2-4 hours, with a maximum of 4 doses. It may make some women feel woozy, forgetful and sick and for this reason you will be offered an anti-sickness drug with it. Pethidine crosses the placenta to the baby and can sometimes make him/her sleepy and slow to breastfeed especially if given too close to the birth. You can use Entonox alongside Pethidine if you wish. If you have pethidine, you are advised not to use the birthing pool for two hours after administration, but it may be possible to return to the pool later if you are not feeling dizzy or unwell.
Epidural
This is an infusion of local anaesthetic through a very small tube in your back and takes away the sensation of pain with contractions. A separate leaflet with in-depth information on epidurals is
available from your midwife or doctor. Epidurals are not available at a homebirth.
Midwives’ advice
Each labour and birth are different. Planning to use, or not use, certain options is not always practical, as individual circumstances and decisions can change once labour starts. This means a flexible approach is sensible. Your Midwife will be able to offer you advice and support you to make informed decisions.
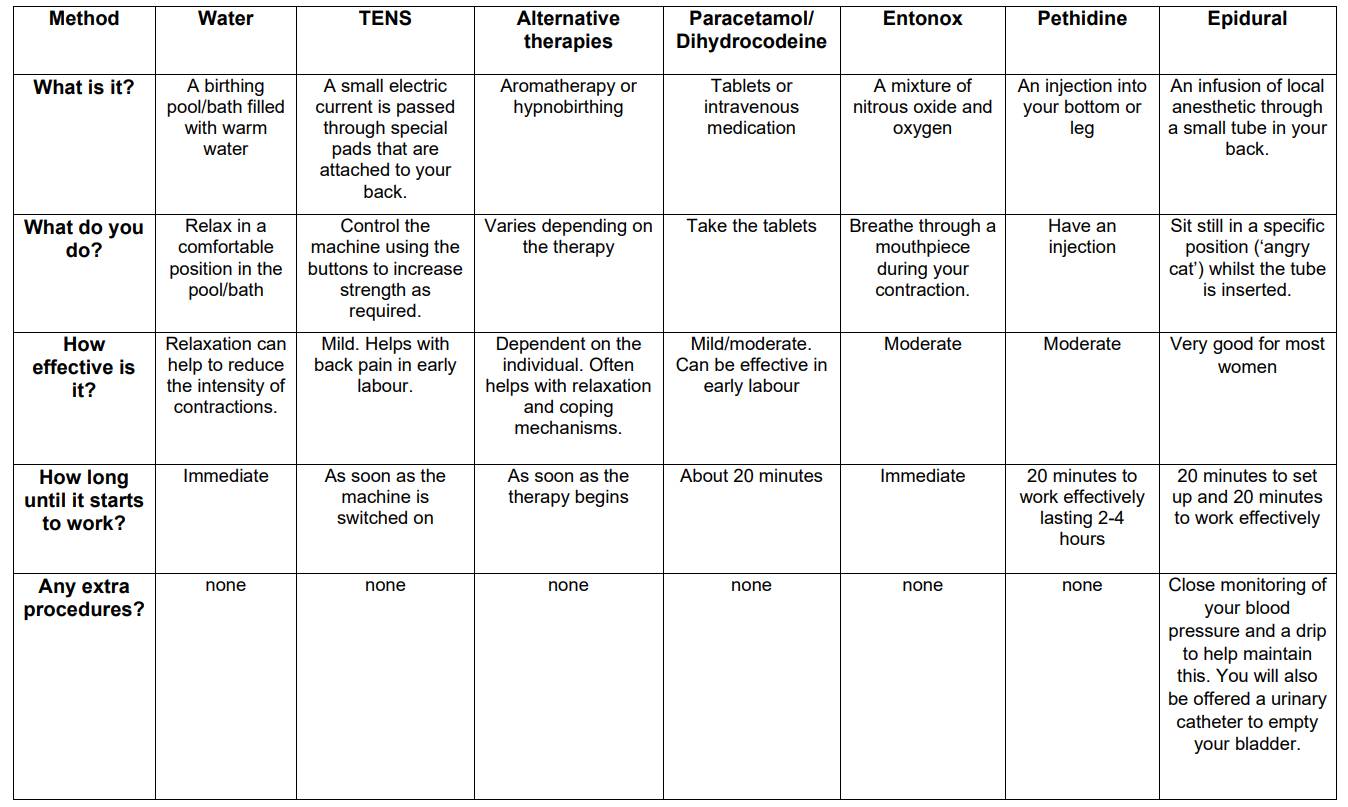
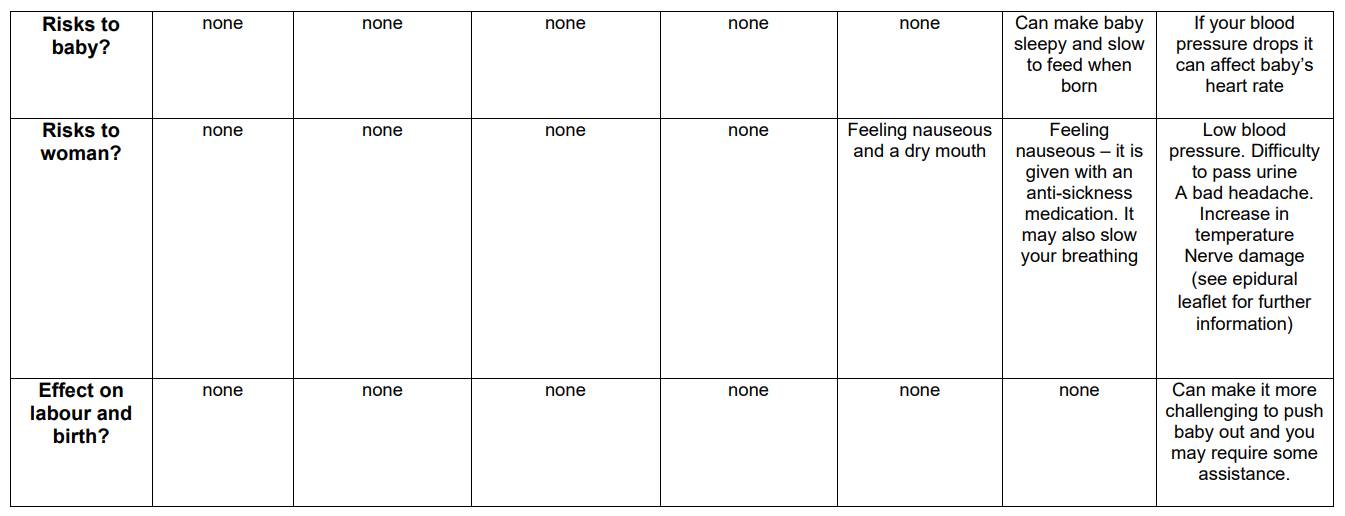
Comparison table (adapted from Obstetric Anaesthetists’ Association)