Sigmoid Colectomy
Please note, this page is printable by selecting the normal print options on your computer.
Introduction
Sigmoid Colectomy is the name given to the operation to remove the diseased part of your bowel. The operation can be done in two ways.
- It can either be performed in the traditional method of opening up the tummy from above your navel (belly button) down in a straight line (approximately 20 centimetres in length). The wound will either be stitched, stapled or glued back together at the end of the operation and will heal in ten to fourteen days in an uncomplicated case.
- Or the operation can be performed laparoscopically. The other names for laparoscopic surgery are keyhole surgery, minimal access surgery or minimally invasive surgery.
A laparoscope is like a thin telescope with a light source. The laparoscope is passed into the abdomen through a small incision (cut) in the skin often referred to as a port. It is used to light up and magnify the structures inside the abdomen. This is then connected to a television monitor so that the surgeon can see clearly inside the abdomen. Fine instruments are then passed into the abdomen through three or four small incisions in the skin. These instruments are used to lift, cut and take a biopsy from inside the abdomen.
The decision of which method is used to perform your operation will always be made with your best interests in mind. However occasionally it is necessary to abandon laparoscopic surgery and open up the abdomen if it becomes difficult to proceed safely with laparoscopic surgery.
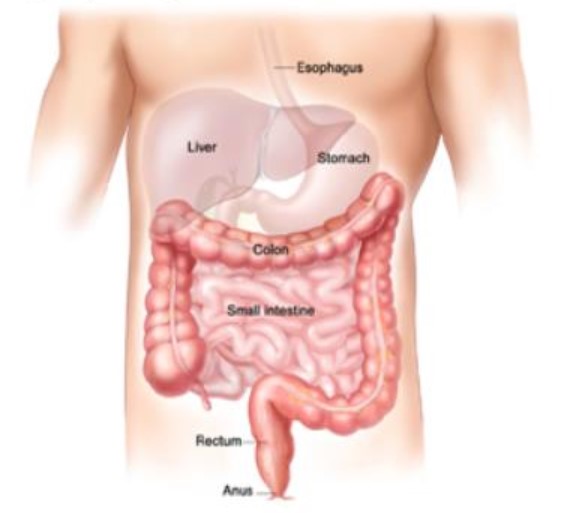
The Large Bowel
The large bowel (intestine or colon) is approximately 1.5 metres long. This part of the digestive tract carries the waste from digested food from the small bowel and gets rid of it as waste through the opening in the back passage (anus).
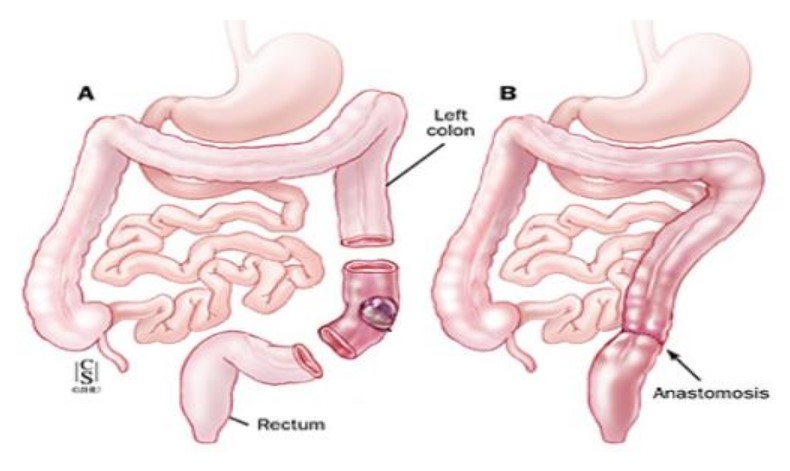
Sigmoid Colectomy
This operation can be done for cancer or diverticulitis. The aim of the surgery is to remove the section of bowel affected by disease. The two cut ends are then joined together as shown in the diagram below. The new join is called an anastomosis.
Sometimes the surgeon wants to protect the new join and give it a longer time to heal. In that situation, your surgeon would bring out part of the small bowel onto the surface of the skin as an ileostomy (stoma). This allows waste from the body to pass out through the abdomen into a stoma bag. The ileostomy would then be closed at a second operation a few months later. If you have an ileostomy you will see the stoma nurse for help and advice and she will give you written information about the ileostomy.
Occasionally, it is not possible to rejoin the bowel at the time of the operation and the bowel would be brought out onto the surface of the skin as a colostomy (stoma). The colostomy allows waste from the body to pass out through the abdomen into a stoma bag. The waste from this part of the bowel is very similar to the waste from your bottom. If you have a colostomy you will see the stoma nurse specialist for help and advice and she will give you written information about the colostomy.
If you would like more information about this before your operation please contact the stoma nurse on 01908 996951.
Risks of this operation
Any operation carries a risk, the risks of all operations include:
- Chest Infection. This would require antibiotics and physiotherapy.
- Blood Clots in the legs (deep vein thrombosis) or in the lung (pulmonary embolism). We decrease this risk by using elastic stockings and blood thinning injections.
- Anaesthetic this operation is carried out under a general anaesthetic (you will be asleep). If you would like an explanation sheet about general anaesthetics and the associated risks please ask for one. If you are at increased risk because of other medical problems you may have your consultant will refer you to an anaesthetist for a formal assessment.
- Bleeding. This can occur with any operation.
- Patients who are very overweight, smoke or have other medical problems are at increased risk of all of these complications.
This is a major operation that has serious risks of which a small number of people do not survive. Your consultant will discuss your individual risks with you and answer any questions you have. Measures are taken to reduce these risks; however it is not possible to stop all risks completely.
The risks of this operation also include:
- Leakage at the anastomosis (new join in the bowel). This is a serious complication. It is treated with antibiotics and often requires further surgery which may result in a stoma (as discussed previously). The stoma specialist can give you more information on this and will see you in hospital if this complication occurs.
- Increased risk of infection because the bowel is an organ that is full of bacteria. This may be in the form of a wound infection or an infection inside the abdomen in the form of an abscess. Antibiotics are given to help control the infection and sometimes drainage of an abscess is necessary.
- Bowel stops working. This is temporary but can cause bloating of the tummy and sickness.
- Damage to other internal organs whilst removing the diseased bowel in particular the bladder and small tubes to the bladder from the kidneys.
Risks of not having the surgery
Just as there are risks of having surgery there are also risks of not having surgery. These include:
- Symptoms such as pain and bleeding becoming worse
- If the operation is done for cancer, the cancer will spread to other organs
- The bowel fistulae (form a new tract to another organ in your body) or even burst which could lead to further complications and may need surgery
Preparation for surgery
Before surgery the bowel may need to be cleaned out (if the consultant feels this would be useful). You may be given a strong laxative to drink that will cause you to have diarrhoea. This will be given the day before your operation. You will not be allowed anything to eat but you may drink clear fluids (that is fluids with no food or milk). Your letter will inform you when you have to stop eating and drinking in preparation for your anaesthetic.
The stoma nurse will see you the morning of your operation and discuss with you the possibility of a colostomy and where on your tummy the stoma would need to be placed. A mark (with pen) will be made showing the surgeon where to place the stoma should it be necessary.
It is important to mark this position to make sure the stoma would be placed in a suitable position for you to manage.
If you have been told you are to follow the enhanced recovery programme please read the enhanced recovery information sheet as some information will be different.
Enhanced recovery is a way of preparing you for surgery so that your stay in hospital is as short as possible.
After surgery
The recovery period after bowel surgery varies. It usually involves a stay in hospital from three to ten days (in uncomplicated cases) depending on whether you have had open or laparoscopic surgery.
Immediately after your operation the following tubes may be in place to help us care for you:
- Pain control will be administered through either an epidural (tube into your back) or a drip (tube into the veins on your arm). This will help you move around more freely. As you recover these will be removed and pain killers will be given in the form of tablets. The pain gradually eases, particularly once you are up and moving around.
- Fluids in the form of a drip in your arm will keep you hydrated until you are able to drink freely.
- A catheter (tube to your bladder) will drain your urine into a collection bag so we can accurately measure the amount.
- A drain into your tummy-this is a tube to drain fluid away from the operation site. This will be removed when it finishes draining which is usually within two to five days.
These tubes will be removed as soon as possible depending on your recovery. The nursing staff will help you get you out of bed as soon as possible after the operation, being mobile will help to reduce the risk of complications from the operation.
Diet
You may be able to eat during the first few days of recovery but your appetite will probably be reduced. It is important to eat small frequent amounts of easily digested food. In the first few days you will be given specific advice on what you can eat. Meals can be supplemented with nourishing soups and snacks and high energy drinks. The body requires lots of calories during the healing process.
After the first few days there is no special diet and we encourage you to build up to your normal diet as soon as you can tolerate it. However if you have an ileostomy the stoma nurse will give you detailed dietary advice.
Bowel actions
The bowel may take a little while to recover. Passing wind is a sign that your bowel is starting to work again. It is normal for the bowel to be irregular and sometimes is necessary to give medications to either slow the bowel down or give mild laxatives to encourage the bowel to move. This is still relevant if you have a colostomy.
Exercise
You will be encouraged to get out of bed the following day and you will be seen by a physiotherapist who will help you do this. You will be wearing elastic stockings to reduce your risk of a blood clot but moving around will also help. The physiotherapist will also give you deep breathing exercises as this will help prevent chest infections.
Lifting after abdominal surgery is not recommended for approximately six weeks after your operation. If you have a stoma, the stoma nurse will give you detailed advice on lifting.
Stoma care
If you had a stoma formed during your surgery (either a colostomy or an ileostomy) the stoma nurse specialist will see you regularly to give you help and advice on managing your stoma and give you will be given all the equipment you need to do this. You have to be able to manage the stoma without help before you can be discharged home. The stoma nurse will also visit you at home within a few days after discharge to monitor your progress.
Driving
Check with your insurance company about any exclusion they may have. This includes being under the influence of some pain medication. You must be able to perform an emergency stop and you are not excluded from wearing a seat belt.
When you go home
When you go home you may find that on some days you feel better than on other days. It is quite normal to have ‘good’ and ‘not so good’ days.
However it is important to contact the GP if any of the following occur:
- Discharge or leakage from the wound or drain site
- High temperature
- Uncontrolled shivering/feeling hot then cold
- Pain when passing urine/frequent need to pass urine or very offensive smelling urine
- Difficulty with breathing, chestiness or cough with green or yellow phlegm
- Pain in the calf, leg or chest
- Abdominal pain which is different from the usual post operative soreness
- Bleeding from the back passage
- Vomiting
Results of your operation
The piece of bowel that is removed is sent to the laboratory for detailed testing. The results will take ten to twenty days to be processed and a report will be sent to your consultant. Your consultant or nurse specialist will then arrange an appointment to discuss with you the results.
Confidentiality
As part of your treatment some kind of photographic record may be made. For example, photographs or video. You will always be told if this is going to happen. The photograph or video will be kept with your notes and will be held in confidence as part of your medical record. This means that it will only be seen by those involved in providing care for you or by those needing to check the quality of care you have received.
The use of photographs and video is also extremely important for other NHS work, such as teaching or medical research.
If we would like to use the information for these purposes we would only do so with your permission. We do not use any information in a way that identifies you.
This information leaflet is to support and not to replace discussion between you and your specialist.
Before you give your consent to any treatment you should raise any questions you have with your specialist.
- Stoma Nurses – 01908 996951
- Colorectal Nurses – 01908 996953
- Enhanced Recovery Nurse – 01908 996540
Please leave a message on our answer machine if we are not in the office.
