Sacrocolpopexy for Vault Prolapse
Please note, this page is printable by selecting the normal print options on your computer.
What is a vaginal vault prolapse?
• Prolapse occurs when the pelvic floor muscles and the vaginal walls are weak. A vaginal vault prolapse is prolapse arising from the top of the vagina (vault) where the uterus (womb) was situated.
• Prolapse usually occurs after childbirth but is most noticeable after the menopause when the strength of supporting tissue deteriorates.
• The apex is the deepest part of the vagina (top of it) where the uterus (womb) usually is located. If you have had a hysterectomy then the term (vault) is used to describe the area where your womb would have been attached to the top of the vagina. A vaginal vault prolapse is a prolapse arising from the vaginal vault (see diagram below).
Figure 1. A diagram, sideways on, showing the normal anatomy (dotted line) and a prolapsing vaginal vault (continuous line)
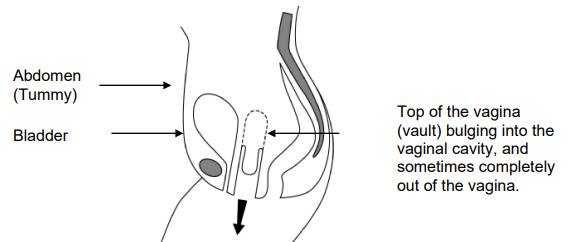
• It may be accompanied by a posterior vaginal wall prolapse, either a high posterior vaginal wall prolapse called an enterocele (containing bowel), or a low posterior vaginal wall prolapse called a rectocele (containing rectum), or sometimes both, or an anterior vaginal wall prolapse called a cystocele (containing the bladder).
• The pelvic floor muscles are a series of muscles that form a sling or hammock across the opening of the pelvis. These muscles, together with their surrounding tissue, are responsible for keeping all of the pelvic organs (bladder, uterus, and rectum) in place and functioning correctly.
• With straining, for example on passing a motion, the weakness described above allows the vault of the vagina to bulge downwards and the rectum (back passage) to bulge into the vagina and sometimes bulge out of the vagina.
• Some women have to push the bulge back into the vagina with their fingers in order to empty their bladder or complete a bowel movement. Some women find that the bulge causes a dragging or aching sensation.
What is sacrocolpopexy?
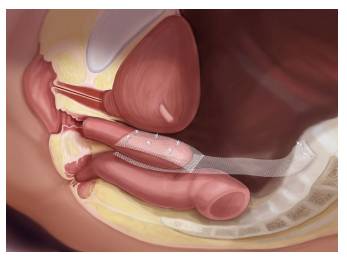
• In this operation the top of the vagina (vaginal vault) is suspended to a prominent part of the back bone (the sacral promontory) via a piece of synthetic mesh.
• Success of this operation is approximately 90%.
• This operation has been performed for a long time.
• It can involve a cut on the abdomen (tummy) and/or can be done through keyhole surgery.
How the operation is performed – sacrocolpopexy
• The operation is done under general or spinal anaesthetic.
• A general anaesthetic will mean you will be asleep (unconscious) during the entire procedure.
• The legs are placed in stirrups (to elevate them).
• A horizontal or bikini incision is made in the lower abdomen (tummy). The operation can sometimes be done via keyhole surgery which means quicker recovery.
• The prolapse is pushed up from below.
• A synthetic mesh is sutured (stitched) to the top, back and sometimes the front of the vagina and the other end is sutured or stapled (titanium staples) to a prominent part of the back bone (the sacral promontory) internally.
• The mesh remains permanently in the body.
• This effectively suspends the vagina via the graft to a sturdy bone.
• A urinary catheter will be left in place overnight.
What are the risks?
General risks
• Anaesthetic risk. This is very small unless you have specific medical problems. This will be discussed with you.
• Haemorrhage. There is a risk of bleeding with any operation. The risk from blood loss is reduced by knowing your blood group beforehand and then having blood available to give you if needed. It is rare that we have to transfuse patients after their operation. Please let your doctor know if you are taking an anti-clotting drug such as warfarin or aspirin.
• Infection. There is a risk of infection at any of the wound sites. A significant infection is rare. The risk of infection is reduced by our policy of routinely giving antibiotics with major surgery.
• Deep vein thrombosis (DVT). This is a clot in the deep veins of the leg. The overall risk is at most 4-5% although the majority of these are without symptoms. Occasionally this clot can migrate to the lungs which can be very serious and in rare circumstances it can be fatal (less than 1% of those who get a clot). DVT can occur more often with major operations around the pelvis and the risk increases with obesity, gross varicose veins, infection, immobility and other medical problems. The risk is significantly reduced by using special stockings and injections to thin the blood (heparin).
Specific risks of sacrocolpopexy
• Damage to local organs. This can include bowel, bladder, ureters (pipes from kidneys to the bladder) and blood vessels. This is a rare complication but requires that the damaged organ is repaired and this can result in a delay in recovery. It is sometimes not detected at the time of surgery and therefore may require a return to theatre. If the bladder is inadvertently opened during
surgery, it will need catheter drainage for 7-14 days following surgery. If the rectum (back passage) is inadvertently damaged at the time of surgery, this will be repaired, however, inserting the mesh may be delayed till a later date. This will require another operation, and in rare circumstances, a temporary colostomy (bag) may be required.
• Prolapse recurrence: if you have one prolapse, the risk of having another prolapse sometime during your life is 30%. This is because the vaginal tissue is weak. The operation may not work and it may fail to alleviate your symptoms.
• Pain: general pelvic discomfort usually settles with time. Tenderness on intercourse due to vaginal tethering may occur. Occasionally pain on intercourse can be permanent.
• Mesh exposure/extrusion occurs when the plastic mesh protrudes through the vagina (incidence of around 10%). This may require a repeat operation to trim the mesh and in severe cases may compromise the operation.
• Infection of mesh: the mesh and/ or the tissues attached to it (vagina and back bone) may get infected. This is usually treated by antibiotics and in rare cases, by removing the mesh.
• Change in bladder and bowel function: changing the axis of the vagina might interfere with the voiding/ continence mechanism leading to voiding dysfunction, or worsening or new urinary incontinence. If you experience this, please let us know as this can be treated. Some patients experience worsening constipation following surgery. This may resolve with time. It is important to try to avoid being constipated following surgery to reduce prolapse recurrence.
• Reduced sensation during intercourse: sometimes the sensation during intercourse may be less and occasionally the orgasm may be less intense.
Does sacrocolpopexy work?
• Success of this operation is approximately 90%
• This operation has been performed for a long time.
What will happen after the operation?
• On return from the operating theatre you will have a fine tube (drip) in one of your arm veins with fluid running through to stop you getting dehydrated.
• You will have a tube (catheter) draining the bladder overnight. The catheter may give you the sensation as though you need to pass urine but this is not the case.
• Usually the drip and catheter come out the morning after surgery or sometimes later the same day. This is not generally painful.
• The day after the operation you will be encouraged to get out of bed and take short walks around the ward. This improves general wellbeing and reduces the risk of clots on the legs.
• It is important that the amount of urine is measured the first couple of times you pass urine after the removal of the catheter. An ultrasound scan for your bladder may be done on the ward to make sure that you are emptying your bladder properly. If you are leaving a significant amount of urine in your bladder, you may have to have the catheter re-inserted back into your bladder for a couple of days more or be taught to do self catheterisation.
• You may be given injections to keep your blood thin and reduce the risk of blood clots normally once a day until you go home or longer in some cases.
• The wound is not normally very painful but sometimes you may require tablets or injections for pain relief.
• There will be slight vaginal bleeding like the end of a period after the operation. This may last for a few weeks.
• The nurses will advise you about sick notes, certificates etc. You are usually in hospital for up to 4 days.
After the operation – at home
• Mobilization is very important; using your leg muscles will reduce the risk of clots in the back of the legs (DVT), which can be very dangerous.
• You are likely to feel tired and may need to rest in the daytime from time to time for a month or more, this will gradually improve.
• It is important to avoid stretching the repair particularly in the first weeks after surgery. Therefore, avoid constipation and heavy lifting. The deep stitches dissolve during the first three months and the body will gradually lay down strong scar tissue over a few months.
Avoiding constipation
• Drink plenty of water / juice.
• Eat fruit and green vegetables especially broccoli.
• Plenty of roughage e.g. bran / oats.
• Do not use tampons for 6 weeks.
• There are stitches in the skin wound in the vagina. Any stitches under the skin will melt away by themselves. The surface knots of the stitches may appear on your underwear or pads after about two weeks, this is quite normal. There may be little bleeding again after about two weeks when the surface knots fall off, this is nothing to worry about.
• At six weeks gradually build up your level of activity.
• After 3 months, you should be able to return completely to your usual level of activity.
• You should be able to return to a light job after about six weeks, and a busy job at 12 weeks. Always avoid unnecessary heavy lifting.
• You can drive as soon as you can make an emergency stop without discomfort, generally after three weeks, but you must check this with your insurance company, as some of them insist that you should wait for six weeks.
• You can start sexual relations whenever you feel comfortable enough after six weeks, so long as you have no blood loss. Do expect things to be different, after the operation the vagina will be suspended and therefore under slight tension. It may feel tense if you suddenly move.
• Follow up after the operation is usually six-eight weeks. This is at the hospital by your consultant.
Alternatives to surgery
• Do nothing – if the prolapse (bulge) is not distressing then treatment is not necessarily needed. If, however, the prolapse permanently protrudes through the opening of the vagina and is exposed to the air, it may become dried out and eventually ulcerate. Even if it is not causing symptoms in this situation it is probably best to push it back with a ring pessary (see below) or have an operation to repair it.
• Pelvic floor exercises (PFE). The pelvic floor muscle runs from the coccyx at the back to the pubic bone at the front and off to the sides. This muscle supports your pelvic organs (uterus, vagina, bladder and rectum). Any muscle in the body needs exercise to keep it strong so that it functions properly. This is more important if that muscle has been damaged. PFE can strengthen the pelvic floor and therefore give more support to the pelvic organs. These exercises may not get rid of the prolapse but they make you more comfortable. PFE are best taught by an expert who is usually a Physiotherapist. These exercises have little or no risk and even if surgery is required at a later date, they may help your overall chance of being more comfortable.
Types of pessary
• Ring pessary – this is a soft plastic ring or device which is inserted into the vagina and pushes the prolapse back up. This usually gets rid of the dragging sensation and can improve urinary and bowel symptoms. It needs to be changed every 6-9 months and can be very popular; we can show you an example in clinic. Other pessaries may be used if the Ring pessary is not suitable. Some couples feel that the pessary gets in the way during sexual intercourse, but many couples are not bothered by it.
• Shelf pessary or gellhorn – If you are not sexually active this is a stronger pessary which can be inserted into the vagina and needs changing every 4-6 months.
Reference
The information in this leaflet is based on British Society of Urogynaecologist information leaflet: Sacrocolpopexy For Vault Prolapse https://bsug.org.uk/
Other sources of information and help:
Bladder & Bowel Foundation,
SATRA Innovation Park, Rockingham Road
Kettering, Northants, NN16 9JH
Nurse helpline for medical advice: 0845 345 0165
Counsellor helpline: 0870 770 3246
General enquiries: 01536 533255
Fax: 01536 533240
[email protected]
http://www.bladderandbowelfoundation.org
http://pogp.csp.org.uk/publications/pelvic-organ-prolapse-physiotherapy-guidewomen
Sacrocolpopexy:
http://www.nice.org.uk/guidance/index.jsp?action=download&o=42887
Hysterectomy and Sacrocolpopexy:
http://www.nice.org.uk/guidance/index.jsp?action=download&o=42894
http://www.easyhealth.org.uk/
