Referral to Fetal Medicine Unit (FMU)
Please note, this page is printable by selecting the normal print options on your computer.
You have been referred for further assessment of your baby following your scan today. The Fetal Medicine Unit (FMU) is made up of a team of doctors and midwives who specialise in the medical care of babies before they are born.
We appreciate that this can be a stressful time whilst awaiting further investigations and diagnosis. The fetal medicine midwives are here to help you through the next steps and ensure you have the information you need to make any ongoing decisions.
The fetal medicine midwives will refer you to be seen by the relevant consultant within an appropriate timeframe. We run fetal medicine clinics at Milton Keynes Hospital and Oxford Hospital. The location of your follow up will depend on availability and the speciality required.
If a member of the team was not available to see you face to face following today’s appointment, they will contact you within 1 working day to discuss the referral pathway and follow up plan.
What to expect at your appointment
At this appointment you will meet the fetal medicine consultant, a doctor who specialises in the medical care and diagnosis of conditions in babies before they are born.
The consultant will ask to complete a scan on your abdomen (tummy) to look at the anatomical features of your baby (the structures and organs that make up your baby).
If the scan findings do not confirm the initial suspicions, you may be discharged from fetal medicine and advised to continue your care with your midwife and/or consultant as before.
Dependant on the scan findings you may be offered additional specialist input. This may be at Milton Keynes Hospital or Oxford Hospital, dependant on the speciality required.
National Congenital Anomaly and Rare Diseases Registration Services (NCARDRS )
Public health England are responsible for improving the health of people across England. They have special permission from the government to collect information to further improve the ways these conditions are treated.
Please click here to read more about why we share information with NCARDRS. If you wish to opt out of information sharing, please let the Milton Keynes fetal medicine team know.
Prenatal Diagnostic Testing
Some scan findings raise suspicions of an underlying genetic condition. If the fetal medicine consultant has identified any of these features, they may offer you prenatal diagnostic testing (a sample of the cells of your placenta or amniotic fluid, looking at the chromosomes for genetic information).
The type of test offered depends on how many weeks pregnant you are. Please take the time to read about both Chorionic Villus Sampling (CVS) and an Amniocentesis.
Testing is not mandatory and is your choice. We are here to provide you with the information and support your decision.
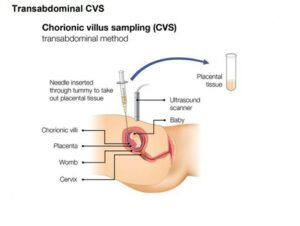
Chorionic villus sampling (CVS)
This involves taking a tiny sample of tissue from the placenta (placental tissue) for testing. The sample contains some of your baby’s cells which contain genetic information (DNA). CVS is usually done from weeks 11 to 14 of pregnancy but can be done later. If the doctor decides it is not safe to do the procedure at a particular time, they may offer you another appointment 7 to 14 days later when the placenta will be larger and easier to reach.
Your abdomen (tummy) is cleaned with antiseptic and we will inject local anaesthetic to numb a small area of the skin. A fine needle is inserted through your abdomen, into your uterus (womb) and into the placenta to take the sample. An ultrasound probe is used to guide the direction of the needle throughout the procedure.
In rare cases, less than 1 in 100 cases, an unusual result is obtained due to a rare condition call placental mosaicism. This is where the sampled DNA from the placenta is not the same as the baby’s DNA. In these cases, we may offer an amniocentesis to verify the baby’s DNA.
A CVS cannot test for spina bifida or other physical differences. It cannot detect conditions such as autism or cerebral palsy.
It can occasionally find an unexpected chromosome change which is unrelated to the ultrasound findings.
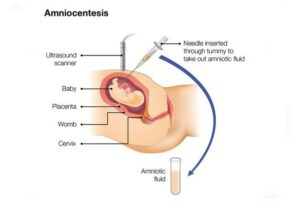
Amniocentesis
This is when we take a small amount of amniotic fluid (the water around your baby inside your uterus) for testing. The sample contains some of the baby’s cells, which contain genetic information. Amniocentesis is usually done between 15 and 24 weeks of pregnancy, or after 32 weeks of pregnancy.
We clean your abdomen (tummy) with antiseptic and insert a fine needle through your abdomen and into your uterus (womb) to take the sample. An ultrasound probe is used to guide the direction of the needle throughout the procedure.
An amniocentesis cannot test for spina bifida or other physical differences. It cannot detect conditions such as autism or cerebral palsy.
It can occasionally find an unexpected chromosome change which is unrelated to the ultrasound findings.
Preparation for CVS or Amniocentesis
You can eat and drink as normal before and after the procedure. Please come to the appointment with a comfortably full bladder as this will allow your uterus (womb) to rise, which will make it easier to check the position of your baby and placenta.
We will need to have your blood results available prior to performing diagnostic testing. These tests would have been completed at your initial midwife appointment. It is important for us to know your blood group and if there are any known infections such as HIV, Hepatitis B or Syphilis.
If your blood group is Rh Negative, we will discuss giving you an injection called Anti D after the procedure. Anti D is a medicine made from blood products to prevent the development of antibodies that could cause problems for future pregnancies.
We ask to take a blood sample from you and the father of the baby to accompany the CVS or amniocentesis to the laboratory. If a change in the baby’s chromosomes is found, then this can help the laboratory in detailing the significance of the change and the reoccurrence risk (how likely the condition is to occur in future pregnancies).
It is possible that we collect maternal cells as well as the baby’s cells during sampling, this is called maternal cell contamination. The laboratory will use the maternal blood sample to ensure the baby’s cells are tested correctly.
Possible risks of CVS and Amniocentesis
Most women say that a CVS or amniocentesis is uncomfortable rather than painful. Some say it feels like period pain. You may feel anxious before and after the test. You may notice some cramping for a few hours afterwards. This is normal. You can take paracetamol for any discomfort. You do not need to rest or stop driving after the procedure.
It is not always possible to get a result from the first CVS or amniocentesis. Up to 6 in 100 women (6%) will be offered a second procedure.
One in 200 women who have a CVS or amniocentesis will miscarry. We do not know why some women miscarry after these procedures. Most miscarriages happen within 3 days of the procedure, but they can happen up to 2 weeks afterwards. There is nothing you can do to prevent a miscarriage after a CVS or amniocentesis.
There is a risk of less than 1 in 1,000 that CVS or amniocentesis will cause a serious infection. You should call maternity triage or attend A and E, straight away if you experience any of the following symptoms:
- constant or severe pain
- a high temperature of 38°C (100.4°F) or more
- chills or shivering
- heavy vaginal bleeding
- discharge or clear fluid from the vagina
- contractions
Multiple pregnancies
CVS or amniocentesis in twin pregnancies is more complicated and is offered at Oxford Hospital as it is a more complex procedure and may require more than one consultant to be present.
With CVS there is a small chance of getting 2 samples from the same baby, which could give misleading results. The risk of miscarriage when having CVS and amniocentesis with twins is about twice as high as in single pregnancies. If this occurs, it may lead to the miscarriage of both babies.
Results
You can choose whether to receive the results by phone or come into the hospital again and receive the results face-to-face.
In most cases the result will let you know, one way or the other, whether your baby has the condition the test was looking for.
Occasionally the laboratory cannot provide a result within the expected timeframe. This is because the cells may need time to grow before the DNA can be extracted and a result can be obtained.
The first result received is called a QFPCR or RAPID test and usually takes up to 4 working days. The laboratory tests the most common three trisomy conditions first. This result will show if your baby’s chromosomes are positive for Down’s syndrome (Trisomy 21), Edwards syndrome (Trisomy 18) or Patau’s syndrome (Trisomy 13).
In some cases, further testing may be required on the sample. It will depend on the scan findings and the tests requested by the fetal medicine consultant who performed the CVS or amniocentesis. If they have requested a full array, the laboratory will continue to grow the cells and extract DNA to analyse the 23 pairs of chromosomes. This result takes approximately 2 -3 weeks from the date of sampling.
Should you wish to discuss your results further at any point, you can contact the fetal medicine department.
Milton Keynes University Hospital
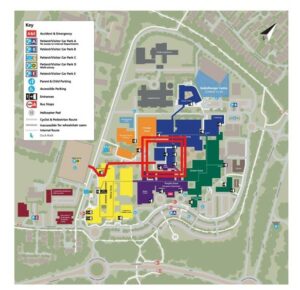
If you have been booked a Fetal medicine appointment in Milton Keynes, park in the multistorey car park, car park D.
Walk to the left of the main entrance, on the outside of the building towards breast care and the treatment centre. Enter the hospital by the blue zone. Antenatal clinic is on your left-hand side.
Fetal Medicine Unit located in Antenatal clinic, Milton Keynes Hospital, Standing Way, Eaglestone, MK6 5LD
Tel: 01908997579 (Mon-Fri 08:00 – 16:00)
Oxford University Hospital
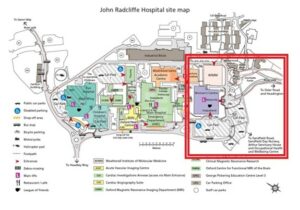
If you have been referred to Oxford Fetal medicine, they will contact you directly within 2 working days with an appointment date and time.
The address will take you directly to Oxford University Hospital. Follow the map directions to park in car park 2. Please allow additional time for parking.
Enter the Women’s Centre and use the lift to access level 6.
Oxford team will inform the Milton Keynes fetal medicine team of the scan findings and the consultant recommendations.
Fetal Medicine Unit, John Radcliffe Hospital, Level 6 of the Women’s Centre, Headley Way, Oxford, OX3 9DU
Tel: 01865221716 (Mon-Fri 08:30 – 17:30)
Support groups and useful websites ARC: Antenatal results and choices https://www.arc–uk.org
Soft UK: Support organisation for trisomy’s
www.soft.org.uk/understanding–chromosomes
FASP: Fetal abnormality screening programme
Screening in pregnancy: CVS and amniocentesis information for parents – GOV.UK
