Preterm birth clinic
Please note, this page is printable by selecting the normal print options on your computer.
Why have I been referred to Preterm birth prevention clinic?
You have been identified by your midwife or obstetrician as being at increased risk of preterm birth. Overall, most maternity service users (over 90%) spontaneously give birth to their baby after 37 weeks of pregnancy, called term delivery. Around 8% of pregnant people spontaneously give birth to their baby preterm before 37 weeks of pregnancy. Most babies born preterm do well, but a few have long term problems.
Most people who come to the Preterm Prevention Clinic will have a full-term pregnancy without the need for any treatment or intervention
This information leaflet will explain:
- what is known about some of the causes of preterm labour
- why service users may be at an increased risk
- what investigations, monitoring and support we can offer you in the clinic.
The reason we would like to offer investigations and monitoring is because treatment can be provided if tests show that it is needed.
What is the Preterm birth prevention clinic?
The clinic provides extra care for service users who have a higher risk of spontaneous early preterm (premature) birth (between 24 and 34 weeks of pregnancy) or second trimester miscarriage (pregnancy loss between 14 and 24 weeks of pregnancy). The clinic is led by consultant obstetricians with an interest in preterm birth prevention.
The Preterm Birth Clinic is for service users who have an increased risk of delivering their baby preterm such as:
- Previous spontaneous preterm birth before 34 weeks or late miscarriage (over 16 weeks gestation).
- Surgery on their cervix (neck of the womb). For example, two or more large loop excisions of the transformation zone (LLETZ) (a common treatment for abnormal cervical cells) or one cone biopsy.
- Surgery to their womb. For example, resection of a uterine septum or treatment for Ashermann’s syndrome.
- Their womb is an unusual shape. For example, bicornuate, unicornate, uterus didelphys.
- Their cervix has been found to be shorter that normal by ultrasound.
- They have had a stitch placed in their cervix (cervical cerclage) in a previous pregnancy or in this pregnancy.
- Previous caesarean section at full dilatation.
At your appointment
You will be seen by Miss Nizami or Mr Patel, consultants obstetricians with interest in preterm birth. They will take a detailed history and review your previous notes and scans. There are three main tests that you will be offered:
- Vaginal swab & urine test: At your first visit we offer pelvic swabs to look for infections such as bacterial vaginosis. These infections are not common, but service users who have them have a higher risk of preterm birth and may benefit from treatment. We also test your urine for infection.
- Cervical length scan: We measure the length of your cervix using a vaginal ultrasound scan. This does not increase the risk of you having a miscarriage or going into preterm labour. This is usually offered in the second trimester onwards (after 14 weeks, although this will depend upon your risk and may be started slightly later in your pregnancy) if we feel that you are at risk of having your baby early due to a short cervix. It is normal to feel anxious when you have not had a scan on your cervix before, but we understand this and will explain the process of the scan before we offer this to you. It is important that you have emptied your bladder prior to the scan as this enables us to look at the neck of your womb more accurately. The transvaginal scan is the only way to accurately measure the length of your cervix, an abdominal scan (where the probe is placed on your abdomen) cannot measure the neck of the womb accurately. Prior to the scan, please inform us if you have any allergies, particularly to latex. We usually repeat the scan every 2 weeks until around 24 weeks, however everyone is very different so the plan can vary from patient to patient.
- Fetal Fibronectin test: A simple swab taken internally from the top of the vagina is tested for a protein called fetal fibronectin. The level of fibronectin is used to predict the chance of preterm birth. The result is available within 10 minutes. Sexual Intercourse affects the accuracy of this result. Fetal fibronectin cannot be completed within 24 hours of sexual intercourse.
What care and treatment will I be offered?
- Monitoring: Most service users who attend the clinic do not require any treatment. We offer to see you regularly to monitor the length of the cervix and to provide you with some support throughout your pregnancy. Most people in the moderate risk group can be discharged after two visits, as their cervical length will be reassuring and therefore at low risk of preterm birth. If you are in the high-risk group, you will usually be seen again – the frequency of attendances will be tailored to your needs.
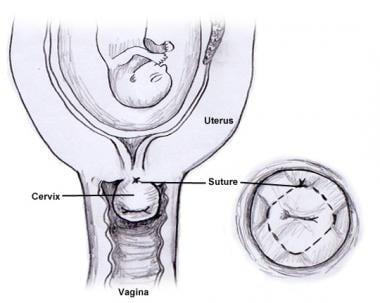
- Cervical stitch: Following regular scans to check the length of the cervix, if your cervix is getting shorter you may be offered a cervical stitch (also known as cervical cerclage or suture). If you have had more than one preterm birth, you may be offered a cervical stitch at approximately 14 weeks to try and prevent another preterm delivery rather than embarking on regular monitoring of the length of the cervix. This is a special stitch which is put around your cervix to keep it closed. This is not beneficial for everyone who attends the clinic but if we feel that this may benefit you, we will discuss this further with you in the clinic and give you some further information. The cervix is reached through the vagina using a speculum. Having a cervical cerclage put in place may mean that the neck of your womb is less likely to undergo changes that can cause it to open. Your baby is therefore held safely inside the womb and your chances of getting an infection or going into labour too early are also reduced. There are some risks to the procedure and not everyone will benefit. We will discuss with you whether cervical cerclage may benefit your pregnancy.
- Progesterone: This is a hormone that plays a role in maintaining pregnancy. There is some evidence to support the use of progesterone to treat a cervix which is shortening. Most recently a large study in the UK showed that progesterone did not help to improve the outcomes of babies born too early when their mother had a short cervix in pregnancy but further studies are ongoing.
- Steroids: If you are more than 24 weeks pregnant and we think that there is a very high chance that you may deliver in the following week, you will be advised to stay in hospital and you may be offered a course of two steroids injections usually over a 24 hour period. Steroids help with your baby’s lung development to reduce the chance of respiratory problems caused by being born early. You will usually only require one course of steroids, so it is important to time them correctly.
Common Questions
- Can I exercise during my pregnancy?
There is no risk associated with starting or continuing moderate exercise during pregnancy. Any sport that may cause abdominal trauma, falls or excessive joint stress should be avoided. - Can I have sex during my pregnancy?
There is no evidence that having sex causes preterm birth. However, we would advise you not to have sexual intercourse:- If your placenta is low-lying. Once the placenta has moved away later in pregnancy it may be safe to resume sexual intercourse – await advice from your obstetrician or midwife
- If you have vaginal bleeding
- If you have had a cervical cerclage placed – avoid intercourse until you have been seen again in the Preterm birth Prevention Clinic.
- 24 hours prior to your obstetric appointment in case a fetal fibronectin is required
- How can I help myself?
- Smoking – we know smoking doubles the risk of preterm birth and we advise smokers to stop smoking immediately. Getting professional help increases the chance that you will stop smoking. Your midwife can provide support and arrange a referral to the smoking cessation services. There are benefits even if you stop smoking in the middle of pregnancy.
- Douching – douching (rinsing) your vagina interferes with the vagina’s normal self-cleaning and with the natural healthy bacteria living in the vagina. Douching is associated with bacterial vaginosis and may increase the chance of preterm birth. We advise you not to douche your vagina.
- Diet – some diets are associated with a lower risk of preterm birth, although the evidence is unclear. Eating a diet rich in vegetables, fruits, oily fish, water as beverage, whole grain cereals and fibre rich bread is beneficial. Increasing the intake of omega-3 long-chain polyunsaturated fatty acids in the diet before 20 weeks of pregnancy either by eating oily fish regularly or in a supplement (500mg-1g per day) has been linked to a lower chance of preterm birth.
- What should I look out for?
Speak to a midwife if you experience any of the following symptoms:- increasing watery vaginal discharge
- increasing abdominal pain
- vaginal bleeding
- increasing feeling of pressure on your vagina.
For non-urgent queries please contact the preterm specialist midwife for on 01908 997 579.
For any of these symptoms or other urgent care needs please call Maternity triage (open 24 hrs) on 01908996483
Further information and support
