Patient handheld Systemic Anticancer Therapy (SACT) booklet
Please note, this page is printable by selecting the normal print options on your computer.
24 HOUR TELEPHONE ADVICE FOR UNWELL PATIENTS 01908 660033 Bleep 1090.
Tumour marker required day 1 of each cycle ……………… (Affix patient label)
IMPORTANT PATIENT INFORMATION
If you have a temperature over 37.5oC, or feel unwell with or without a temperature you must contact the 24 hour Acute Oncology Telephone Advice Service by calling 01908 660033 and ask for bleep 1090 (See your Acute Oncology Leaflet for further information about the service). When you commence your anticancer therapy you should monitor your temperature at least daily and more frequently if you feel unwell or have been told that you have low white cells or are neutropenic. Please make sure that you have a thermometer at home to do this. You may find it useful to make notes each day of your temperature and any side effects such as episodes of diarrhoea/constipation that you may experience.
Contact details
Be aware of the signs of infection:
Fever
Chills
Feeling unwell
Sweating, especially at night
Loose bowel movements
Redness or inflammation of the skin
Cough or sore throat/mouth
Burning on passing water
You are advised to take your temperature at least three times a day if you are neutropenic and are at home. It is essential that you do this immediately if your temperature is 38.Oc or above on one occasion or 37.5oC or above on 2 occasions half an hour apart, or if you have a normal temperature but you suddenly feel unwell. Most SACT reduces the body’s resistance to fight infection. Please be aware that something which may seem to be a minor illness can develop into something more serious needing hospital treatment. SACT can affect regular medications and they may need reviewing. If you have started any new medication e.g antibiotics, herbal medicines, heart medicines etc, please check with your oncology team or haematology team so they can check chemotherapy will not interfere with the way in which these medicines work.
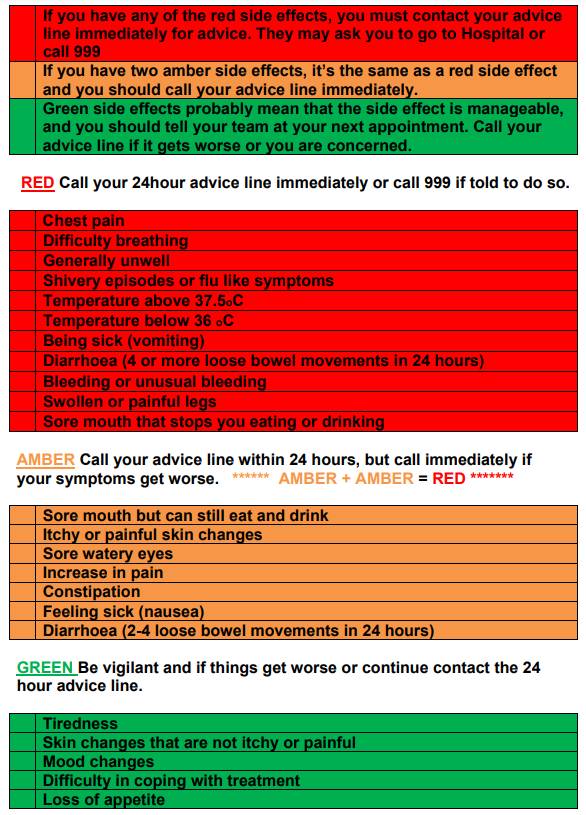
The Traffic Light Assessment: When to call the emergency line 01908 660033 bleep 1090
Traffic Light Assessment
What is chemotherapy?
Chemotherapy is the use of drugs or chemicals to treat illnesses or disease. Most people associate chemotherapy with the treatment of cancer. Many drugs are used to treat cancer. Not all cancers are treated with the same drug or in the same way. Research has helped determine the most effective drugs for different kinds of cancer. You may receive one drug or a combination of drugs. You may receive chemotherapy in addition to other treatments such as, surgery, radiotherapy or biological therapy. Biological therapy or targeted therapies are drugs that mimic substances that occur
naturally in the body to destroy cancer cells. They work by changing the way that cells interact or signal to each other.
What are the benefits of treatment?
The benefits of treatment will depend on the type of cancer you have and how advanced it is. The aims include:
• Intention to cure the cancer; this is when chemotherapy is given to destroy all the cancer cells.
• Reducing the chances of the cancer coming back; for example after surgery, by destroying any cancer cells that are still in the body but are too small to detect. This is often called adjuvant.
• Controlling the growth and spread of the tumour; so that surgery or radiotherapy is easier to perform. This is often called neo-adjuvant.
• Controlling the growth and spread of the tumour; this may slow down its progress and relieve symptoms. This is often called palliative treatment.
What will happen when I arrive at the hospital for my treatment?
This may vary slightly depending on where you receive your drug treatment but on arrival:
• You will book in at reception
• A member of the nursing team will come to meet you at reception and take you through to the clinical area where you will have your treatment.
• You will be given a name band to wear while you are in the ward which will be used to check your identity
To ensure your safety we do the following:
– Your treatment is prescribed
– A pharmacist checks the prescription
– Your treatment is made and checked before it leaves pharmacy, systemic anti-cancer therapies are complex treatments and have to be made in a special prepared suite-this can sometimes cause delays in your appointment in the oncology or macmillan unit.
– Two nurses check your drug
– Two nurses will check your identity before administering the treatment.
How and where will the treatment be given?
Most chemotherapy is given through a drip into a vein in your arm. Sometimes it may be necessary to use a semi-permanent line which is inserted into a major vein e.g. PICC or Hickman line or Porta Cath (if you require such a line this will be discussed with you in more details) Chemotherapy may be given to you by other ways- for example as tablets or using a portable pump.
How will you feel while you are having chemotherapy?
Some chemotherapy drugs have very few side effects and you may be able to carry on living a normal everyday life between visits. Other treatments may be more disruptive. It depends on the type of chemotherapy you are having-each drug is different. Some of the more common side effects of chemotherapy are discussed in the next few pages. More specific side effects to the chemotherapy drugs to be given to you will be an information sheet which will be obtained for you from Macmillan.Org website.
Blood Tests
Your blood will need to be tested each time you visit the hospital for treatment as the medical team need to know that it is normal before they give chemotherapy. Depending on your blood count results, your treatment may have to be delayed. If this happens you will be given another appointment to come back for a further test and, if all is well your chemotherapy. Chemotherapy can affect the bone marrow as all the blood cells are made here. Your doctor or nurse can explain this further to you.
Other tests
The functioning of your organs may need to be checked before your start chemotherapy. Such as:
Heart: Certain chemotherapy drugs can affect the heart and your medical team will ask if you have had any heart problems or high blood pressure. You may have to have a heart trace (ECG) or a heart scan ECHO (Echocardiogram)
Liver: Regular blood tests will monitor how your liver is working.
Kidneys: Regular blood tests will monitor how your kidneys are working.
Sometimes you may be asked to collect your urine (for up to 24 hours) so it can be tested at the hospital.
The effects of chemotherapy on your blood
One thing that all chemotherapy drugs have in common is they tend to lower your resistance to infections. This is because they lower your blood count, especially your white blood count. When you have fewer white blood cells than usual your body is less able to fight infections. This does not mean that you need to isolate yourself from other people, though it is sensible to avoid close contact with those who have obvious coughs, colds, flu and so on. It does mean that you should take it seriously if you develop an infection.
What should you do if you get an infection?
If you develop any of the following while you are on chemotherapy-and for four weeks afterwards-you should ring us for advice immediately on our 24 hour contact number: 01908 660033 Bleep 1090.
A temperature 380C or above on one occasion or above 37.50C on two occasions taken half an hour apart.
A sore throat
A chesty cough
A stomach bug or upset stomach—diarrhoea
A urine infection—stinging or pain on passing urine
Feeling generally unwell, achy or flu like
Redness or discharge around a Hickman or other lines
Shivery episodes after a flushing of a Hickman or other Line.
DON’T DELAY! It is very important to act straight away. Contact us on the 24 hour contact number you have been given.
Other effects of a low blood count
Chemotherapy can also lower your platelet count. Platelets are blood cells which help clot your blood. With most chemotherapy low platelets are unlikely to cause a problem, but if you have unusual bleeding or bruising please let us know. You will be informed if you have low platelets, if you have been advised that they are low please follow the precautions below:
Avoid activities with an increased risk of injury
Use an electric razor
Ladies if you need to shave your legs and underarm please use an electric razor – no wet shaves
Use a soft tooth brush and please do not floss
You may require a platelet transfusion if your platelets are low. Please contact the 24 hour telephone number given to you if you experience any bleeding. Sometimes chemotherapy can also lower your red blood count. This tends to happen slowly over the course of several treatments. A low red blood count can make you feel tired and short of breath. From time to time we offer patient’s blood transfusions to correct a low red cell count when required.
Some of the common side effects of chemotherapy
Nausea and vomiting (feeling and being sick)
Not all chemotherapy drugs will make you feel or be sick. When we use the ones that do, we always given you anti sickness drugs to try and prevent the problem. Improvements in these drugs over the past few year’s means that many patients do not feel sick at all, or only have minor problems. If you are given anti sickness tablets to take for a few days after treatment, do make sure that you take them as prescribed. It’s much better to prevent sickness before it starts.
If despite this you do feel sick after chemotherapy, let us know. We can usually try different anti sickness drugs to help. You could also try ‘sea bands’ these are elastic wrist bracelets which you can buy from your local chemist. They have a small plastic bobble which presses on your anti sickness acupressure point.
Changes to bowel habit
Some chemotherapy drugs can affect the lining of the digestive system and this may cause diarrhoea for a few days. Some drugs may cause constipation and it may be necessary to take laxatives at times in our treatment.
Diarrhoea: Some chemotherapy drugs cause diarrhoea. It usually occurs in the first few days after your chemotherapy. With some chemotherapy drugs it can be quite severe. If you have diarrhoea, remember you can easily become dehydrated. Try to drink plenty of fluids. If you cannot drink enough or if the diarrhoea is increasing you must call the 24 hour contact numbers, it could be a sign of infection.
Hair Loss
Many chemotherapy drugs do not cause hair loss but others cause hair thinning or even complete hair loss, it all depends on which chemotherapy drugs you are having. Your doctors and nurses will be able to tell you how likely hair loss is with your treatment. If it happens, hair loss will usually start about 2-3 weeks after your first chemotherapy treatment. It is important to say that the hair always grows back after the chemotherapy stops.
For some people, the thought of losing their hair temporarily is very upsetting. If you chemotherapy is likely to cause hair loss, we will refer you to Christos Hair Care to arrange a wig fitting for you. Some patients use scarves, turbans or colourful hats to help cope until their hair comes back. Sometimes we can try and reduce hair loss by using ‘scalp cooling’ this means wearing a cold cap on your head 30 minutes prior to chemotherapy, whilst the chemotherapy is administered and then for a period of time after treatment finishes. This is only effective for some chemotherapy and may not be advisable in some cancers—i.e. Haematological cancers. Ask your chemotherapy nurse for more details.
Mouth care
Chemotherapy can affect the lining of your mouth and gums. This, together with a lowered resistance to infection can lead to sore mouths or mouth infection. The inside of your mouth could appear red, inflamed and may bleed. This condition occurs when the mucosal cells that makes up the special tissue that lines the mouth, become red and ulcerated and cause pain or a burning
sensation. This condition is known as mucositis or stomatitis. It is very important to look after your mouth, and inform a nurse if you experience any soreness in the mouth and she can help with providing mouth care treatments.
Changes to your skin and nails
Chemotherapy can sometimes affect your skin in different ways. It may cause dryness and flaking of the skin, patches of darkened skin, and ridges on the nails. It also causes skin to become more sensitive than usual, particularly to sunlight, and your skin will easily burn if exposed to sunlight in summer. It is important to keep covered up when it is sunny, particularly your head, and stay in the shade to help prevent sunburn.
Sore hands and feet
Hand-foot syndrome, or Palmar-Plantar Erythrodysesthesia, is a side effect of some types of chemotherapy and other medicines used to treat cancer. Handfoot syndrome is a skin reaction that occurs when a small amount of the medication leaks out of capillaries (small blood vessels), usually on the palms of the hands and soles of the feet. When the medication leaks out of the capillaries, it can damage the surrounding tissues. Hand-foot syndrome can be painful and can affect your daily living.
Symptoms of hand-foot syndrome include:
• numbness
• tingling, burning, or itching sensation
• redness (resembling a sunburn)
• swelling
• discomfort
• tenderness
• rash
In severe cases of hand-foot syndrome you may have:
• cracked, flaking, or peeling skin
• blisters, ulcers, or sores appearing on your skin
• intense pain
• difficulty walking or using your hands
It is really important that if you have any of these symptoms please inform your nurses at the centre who can discuss with the doctor the best plan for you.
Fertility
It is important that you do not become pregnant or father a child whilst on chemotherapy as the drugs may damage your unborn child. Chemotherapy often makes you temporarily infertile but this can be unpredictable, so it is very important that you continue to use contraception. Sometimes the infertility is permanent. If you are concerned about these ask about sperm storage and egg conservation before the treatment starts. Women who are still having periods may notice changes to their normal pattern. Sometimes the periods may stop or there may be less blood loss. Please do not hesitate to discuss these issues with your Consultant or nurse.
Sex and sexuality
Cancer can affect the way you feel about yourself and your sexuality. You may feel a loss of sexual desire during chemotherapy. Loss of libido (sex drive) is not uncommon in both women and men. However, chemotherapy in itself does not usually affect sexual performance or cause impotence. The stress of your illness or the treatment schedule may make you feel more tired than usual.
Emotional care
The fact you need to have chemotherapy and the effects that it has on you and your life can prompt a range of feelings. Often, talking about your concerns can help you manage them. Please ask a member of the nursing staff if you would like to speak to a Macmillan Cancer and Information Support Nurse.
Taste changes
Patients often tell us that the chemotherapy gives them a strange taste in their mouth. Sometimes food may seem taste less and it is quite common for tea and coffee to taste different. This is usually temporary and your taste should return.
Appetite
There are a few restrictions on what you can eat and drink whilst on chemotherapy. A ‘little of what you fancy’ when you fancy it is always good advice. Alcohol is generally also allowed in moderation. But do check with your nurse or doctor first. Haematology patients should avoid unpasteurised dairy products and take away food and some patients the nurse will ask you to follow a clean food diet. You will be provided with this information.
We would ask you to follow some basic food hygiene guidelines as follows:
Wash hands and protect cuts and wounds before handling food.
Cooked foods should be heated to at least 700C and eaten immediately. Avoid reheating food.
Frozen ready meals can be used if stored and cooked according to the manufacturer’s instructions.
All food should be consumed within the ‘use by’ date
Food should be purchased from clean, reputable shops and stored and cooked according to manufacture instructions
Any food stored in a refrigerator must be covered, and consumed within 24 hours.
Cans of food should be clean and undamaged.
Do not drink from cans or bottles, please use a clean glass or straw
Do not eat foods sold loose for example from a delicatessen, butcher or baker.
Frozen food should be defrosted in a refrigerator.
If you feel you would like to speak to a dietician, please speak to one of the nurses.
Cytotoxic Extravasation
This is a term used when chemotherapy drug leaks out of the vein whilst being injected and can cause irritation. A small number of chemotherapy drugs can cause irritation and tissue damage if they leak out of a vein whilst they are being injected. All nurses who administer chemotherapy have completed training and are fully aware of which drugs are more likely to cause these problems and what to do in the event of an extravasation. Rarely, problems can start after you have left the unit. If you notice any pain, redness, swelling, stinging or burning at the injection site whilst you are having chemotherapy, please tell a nurse straight away, if you experience any problems at home. Please contact the 24 hour contact number you have been given.
Tiredness
Probably the most common side effect of chemotherapy is tiredness. This affects some people more than it does others. If you do feel tired or lethargic, try to balance getting plenty of rest with making sure you carry on with some of your usual activities.
Employment
Returning to work: Many people are able to work throughout their chemotherapy treatment, but it will depend on your treatment and cancer. You should discuss this with your medical team.
Time off work: If you need time off work, your employer may provide sick pay for a limited period of time, or you may be able to claim financial benefits. If you need further information or advice, please ask a member of the team to book you into the Citizen Advice Bureau clinics held in the Macmillan Unit.
Holidays
It is a good idea to discuss with your medical team treating you if you wish to book a holiday, as it may be better to wait until your treatment is finished. It may not be advisable to go abroad until at least one month after your treatment is finished as you can still experience side effects.
What is immunotherapy?
Immunotherapy is a relatively new type of biological therapy which is becoming widely used in cancer patients. It aims to harness the body’s immune response to detect and fight certain cancers.
Our immune system
Our immune systems are made up of organs, cells, proteins and other substances that help protect us from infections and diseases. The immune system is keeping track of all the normal substances normally found in our bodies, it will identify any foreign substances such as germs, viruses, or parasites (antigens) that may appear. Our immune system will react to these foreign substances when an antigen is detected. T Cells are part of our immune system and can kill body cells that have been infected.
How does immunotherapy work?
Cancer occurs when genetic mutations develop in our normal cells leading them to grow inappropriately. Cancer cells produce mutant proteins that our immune system can detect as foreign. However even a strong healthy immune system may have difficulty distinguishing between normal cells and cancerous cells. Immunotherapy increases the ability of our immune system to detect and destroy cancer cells.
There are molecules on T cells that act as ‘a break’ and stop T cells from activating and killing cells. Immunotherapy drugs bind to these molecules and ‘take this break off.’ Therefore rather than targeting the persons cancer cells directly, immunotherapy treatments increase the ability of the immune system to recognise cancels and selectively target and destroy them.
Will I have other drugs as well as immunotherapy?
Immunotherapy may be used as a single agent or in combination with other chemotherapies or radiation.
How will immunotherapy be given?
Immunotherapy is given by intravenous injection. How often you have your treatment will be decided by your consultant, and treatment schedules vary-for example they can be very two or three weeks, or monthly.
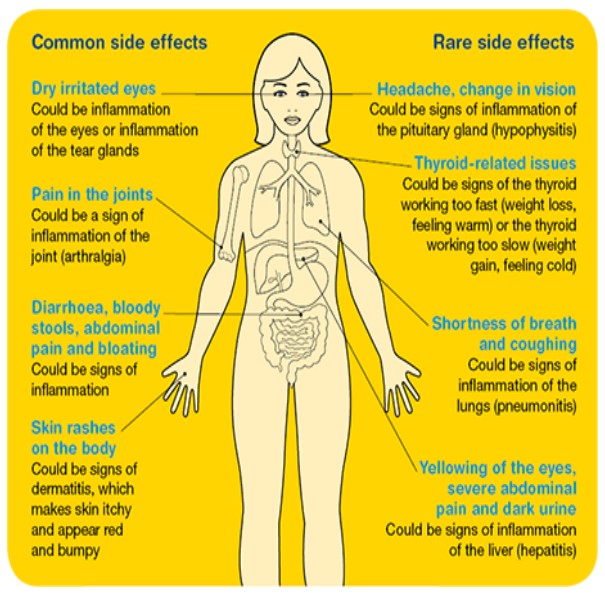
What are the side effects of immunotherapy?
Immunotherapy can cause a wide range of side effects as it can cause inflammation in any organ/part of the body. The side effects of immunotherapy differ from normal chemotherapy so it is
important that you let your doctor or nurse seeing you know that you are on immunotherapy and not chemotherapy for treatment of your cancer. Whilst on immunotherapy there are certain side effects that patients may experience throughout treatment and up to twelve months after. These side effects must be closely monitored by your consultant, specialist nurse and Systemic anti- cancer therapy team. It is important that you as the patient are informed about these side effects and seek appropriate advice as you have been advised at the pre systemic anti -cancer therapy at the start of your treatment.
Please contact Tel: 01908 660033 Bleep 1090 if you experience the following side effects:
General side effects– Tiredness or confusion, shivers, fever, weight gain or loss, a change in behaviour, feeling anxious or irritable
Skin- rashes, itching, yellowing of skin, bruising or bleeding of the skin. Bowels-constipation, diarrhoea or more bowel movements than normal, blood or mucous in stools, black or tarry stools.
Mouth-dry mouth or more thirsty than usual
Head- feeling faint or dizzy, having a persistent headache that will not resolve and is unusual for you.
Throat and chest- worsening shortness of breath, chest pain, rapid heartbeat, developed a new or worsening cough
Muscle joint, or legs- aching muscles, severe or persistent muscle or joint pains, or severe muscle weakness.
Eyes-eyesight has changed from normal to blurred vision, double vision, or any yellowing of the eyes.
Urine-urine colour has changed and peeing unusual amounts, urine is dark in colour.
Nerves-weakness and/or tingling in an arm or leg.
Areas of the body that may be affected by immunotherapy
Targeted therapies
Targeted therapies are drug treatments that interfere with specific features of cancer cells which allow them to grow and spread, although healthy cells can still be affected by these drugs. Targeted therapies work to:
• Stop chemical signals that tell the cancer cell to grow and multiply
• Stop the growth of new blood vessels which may feed the cancer cells
• Change proteins inside the cancer cell so the cell dies or grows more slowly
. Travel Insurance
You may have difficulty obtaining travel insurance, if you wish to go abroad. Within Europe, the E111 has been replaced by the EHIC-European Health Insurance Card. You can register online and you are covered straight away. For more information, visit you’re the Macmillan Information and Support Nurse located within the Macmillan Unit. http://www.fco.gov.uk/en.travel-and-living-abroad/staying -safe/health/
You can apply by post or by phoning an automated service:
Telephone: 03003301350
NHS Business Services Authority
European Health Insurance Card
EHIC applications
Bridge House
152 Pilgrim Street
Newcastle Upton Tyne
NE1 6SN
For more information, visit the Macmillan Unit Information and Support Nurses located within the Macmillan Unit. Or visit the Foreign and Commonwealth Office Website:
http://www.gov.uk/guidance/foreign-travel-checklist
Flu Vaccinations
Can I have the Flu vaccination?
Yes, the flu vaccine is recommended for people who are having chemotherapy or radiotherapy as their treatment may put them at greater risk of getting infections. Patients who are having chemotherapy should ideally be vaccinated at least 2 weeks prior to starting their first cycle of chemotherapy. It is safe to have the flu vaccination between chemotherapy courses; however, it is important not to have the flu vaccination when your immune system is at its lowest. The best time is a couple of days before the next cycle of chemotherapy.
When Treatment finishes
The end of treatment is a time most people look forward too; it can also be a time of anxiety for many. You may wonder ‘what happens next?’ and some people feel they are left with a void after months of their life revolving round treatment. This is a normal feeling. After treatment finishes, you will still be monitored by the doctors and staff. You will receive follow up appointments. Any worries you have can be discussed at your appointments and your family doctor can also be of help. You may not become fully recovered as quickly as you would like. Some people still experience fatigue for some time after treatment, the improvement in this may be slow and hardly noticeable at first.
Non urgent Contact details (For appointments and blood results)
Haematology Patients
Opening Hours 8-6pm Monday to Friday 01908 996351
Oncology Patients
Opening hours 8-6pm Monday to Friday 01908 996431
Alison Sandaver Lead Chemotherapy Nurse Bleep Number 01908 660033 Bleep 1675
