Pain Assessment (A Guide for Parents / Carers)
Please note, this page is printable by selecting the normal print options on your computer.
This leaflet aims to give parents and carers an outline of the ways in which pain is assessed at Milton Keynes University Hospital.
Q – Why is it so important that you assess my child’s pain?
Pain assessments help healthcare professionals to find the most likely cause of your child’s pain and to choose the best way to help relieve it.
Q- How do you assess my child’s pain?
We will ask your child questions (if not possible, we will ask you) about the type, onset, duration, location, frequency of their pain and if anything made the pain better or worse. We will also use a ‘Pain assessment tool’.
Q- What are pain assessment tools?
Pain assessment tools measures pain intensity (how much pain your child is in). There are three main types of pain assessment tools:
– Self-report (what the child says). These are the preferred choice because the child is the one who is actually experiencing the pain.
– Observational (how the child behaves). These can be used with children who are either too young or too distressed to understand and use a self-report tool. They can also be used with children who are cognitively impaired, have communication difficulties or are restricted by bandages or other physical constrictions.
– Physiological (measuring the child’s heart rate, breathing, blood pressure etc.). These are generally used in combination with a self-report or an observational tool.
Q- Why do we use pain assessment tools?
– They help to demonstrate if your child’s pain is getting better or worse.
– They can help determine the success of a pain relieving intervention
– They can give children a method of communicating their pain in a way that adults recognise and consequently, respond to it more promptly.
Q- What Pain assessment tools are used at Milton Keynes Hospital?
The three most common pain tools we use are:
-The Faces pain scale (self-report scale)
– Numeric Pain intensity scale (self-report scale)
– FLACC (observational tool)
Q- Where are these tools kept?
In your child’s bedside folder – please ask your child’s nurse if you cannot find them.
Q- Is it just healthcare professionals that can use these tools with my child?
No, in fact we encourage parents/carers to use these tools with their children. We believe that parents/carers know their children the best and can recognise subtle changes in their child’s manner or behaviour. Children may also find it easier to use the tool with someone familiar.
Q- How do I use these tools with my child?
Below are some simple instructions on how to use the tools. Please speak to a nurse if you would like more information. For all tools try to use language that your child is familiar with, for example some children may be more familiar with the word ‘hurt’ or ‘ouch’ rather than ‘pain’.
The Faces Pain Scale
Most children three to five years and older can use this scale.
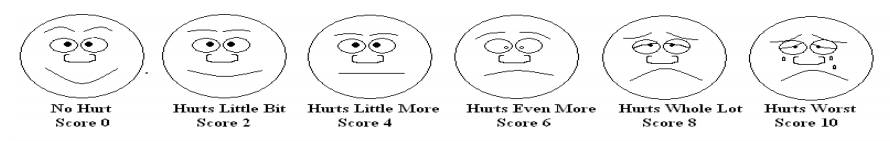
The Faces Pain Scale Instructions
1. Show the faces to your child and say: ‘’these faces show how much something can hurt’’
2. Point to each face and read the words to them. For the Sixth face tell them that you don’t have to be crying to feel this bad’’ (as not all children cry when they are in pain).
3. Then ask your child to point to the face that shows how much pain/hurt they are in.
Numeric Pain intensity scale
To use this scale children need to be able to count and to have some ability to estimate quantities using numbers (often used for children 8 years and older).
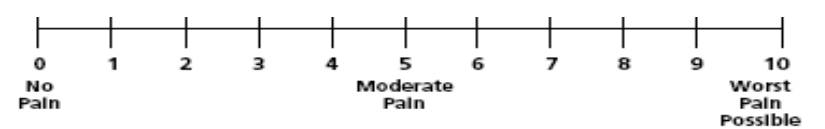
Instructions:
Ask your child the following; ‘’I would like you point to a number on the scale to show me how much pain you are in right now. Zero would mean that you have no pain and ten would mean that you have the worst or most pain’’. This tool can also be used without the scale, for example, your child can just be asked a rating and respond by saying a number or by holding up their fingers to show the number.
FLACC (Faces, Legs, Activity, Cry, Consolability)
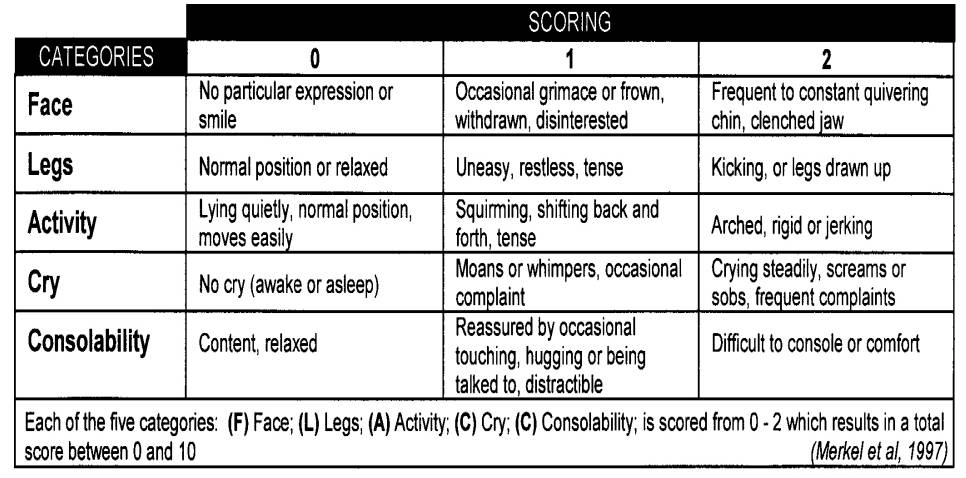
FLACC instructions: Watch your child for one to five minutes and then pick the most appropriate number in each of the five rows and add them up. Scores of four to six out of ten reflect moderate pain. Scores of seven or higher indicate severe pain or discomfort.
Q- Someone suggested that my child keeps a pain diary, what is this?
Pain diaries include regular recordings of the date and time the pain occurred, the pain score, what happened before the pain started and how it was managed. We recommend that you share these diaries with your child’s nurse/doctor, so that they have a better understanding of your child’s pain and are able to treat the pain effectively.
Q- How often will pain assessment tools be used?
– Before and after any pain relieving intervention
– Before, during and after any potentially painful procedures
– When your child’s has their ‘vital signs’ taken such as measuring their heart rate and temperature.
– Other time as and when required e.g. if you sense your child is in pain.
Q- What will the nurses do with the results of my child’s pain assessment?
The nurse will document your child’s pain score on their observation chart and if your child is in pain they will discuss the pain relieving options available with you and your child.
Q- Can we use pain assessment tools at home?
Yes, Yes, Yes! The more you are able to recognise your child’s pain behaviour, the more effective you will become at managing your child’s pain. Using self-report pain tools at home enables your child to communicate their pain in a way in which you can respond effectively, promoting trust and openness with your child. If your child is coming in for a planned operation, we also advise that you practice and familiarise your child with the pain tools before their admission. Otherwise it may be difficult to explain the tools to them when they are still sleepy from their operation!
Pain Management Advice for At Home
‘My Child is in Pain’ is an interactive resource for parents who want to know how to help manage their child’s pain after surgery. It is available via a dedicated webpage: www.mychildisinpain.org.uk, Facebook and You Tube.
“Achy Penguin” is an interactive app that also can be used if your child is in pain.
We hope this leaflet has helped you. If you have any further questions please speak to your child’s nurse/doctor.
