Outpatient Hysteroscopy – An Internal Examination of Your Womb
Please note, this page is printable by selecting the normal print options on your computer.
What is a hysteroscopy?
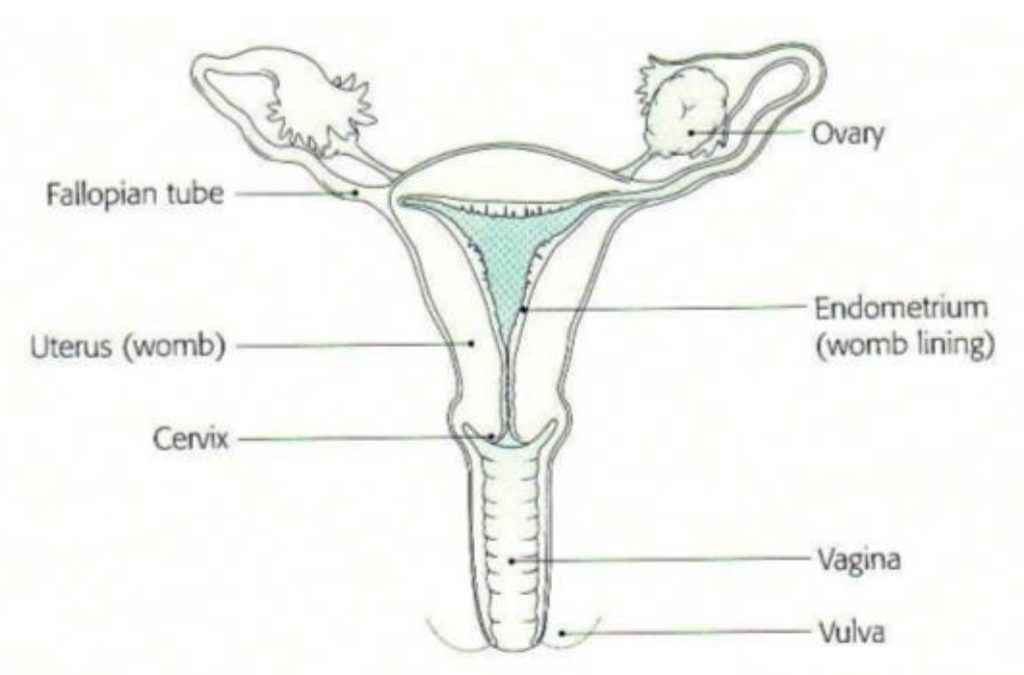
A hysteroscopy is a procedure which uses a fine telescope, called a hysteroscope, to examine the lining and shape of the uterus (womb cavity). It is performed either in the outpatient department or in theatre as a day patient.
What are the benefits of having a hysteroscopy?
A hysteroscopy can help to find the cause of problems relating to:
- Heavy or irregular bleeding between periods
- Bleeding between periods
- Irregular bleeding whilst you are taking HRT
- Irregular bleeding on Tamoxifen
- Bleeding after sexual intercourse
- Bleeding after menopause
- Persistent discharge
- Scar tissue in the womb
- Infertility
- Retrieval of lost Coil
Before your Hysteroscopy
- Ensure you have had an ultrasound scan of the Pelvis prior to the hysteroscopy appointment
- You can eat and drink as normal and take your usual medicines
- We recommend that you take pain relief 1 hour before your appointment 1000mg (2 tablets) Paracetamol or 400mg (2 tablets) ibuprofen this will help prevent any period-type discomfort during and after the procedure
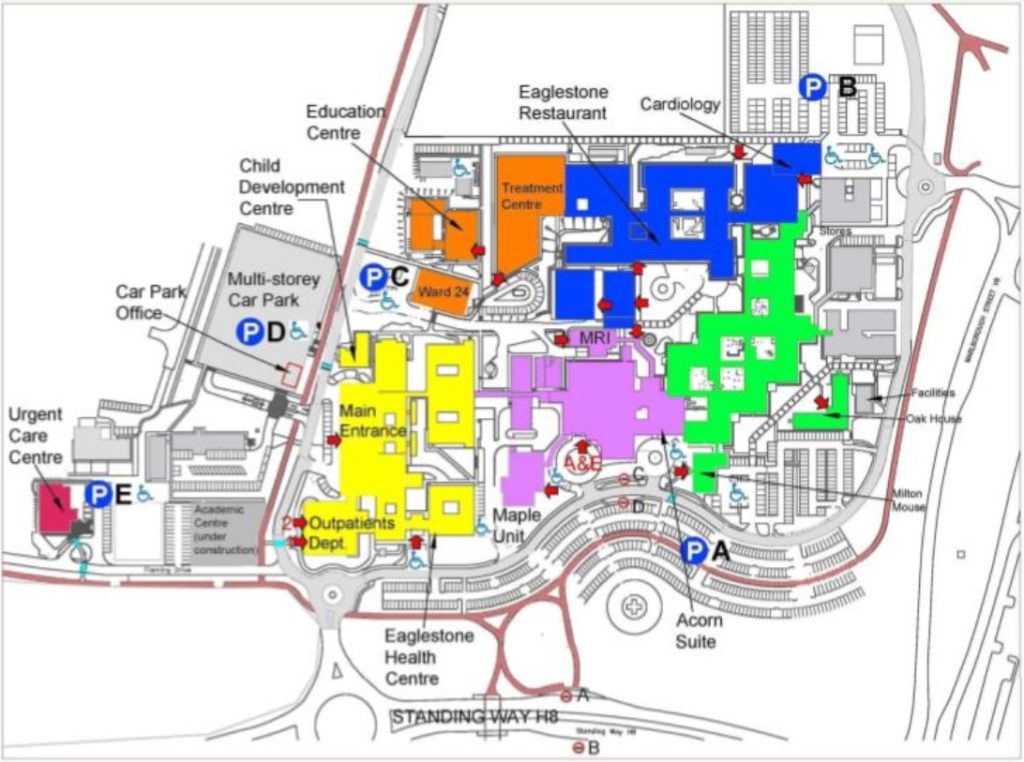
- On arrival you should book in at reception for the Hysteroscopy Clinic
You should ensure that there is no chance of pregnancy prior to the hysteroscopy. You can do this by making sure you use barrier contraception (condoms or a diaphragm) from the first day of your last period before the hysteroscopy right up until the day of the appointment itself. On the day of the procedure we will ask your permission to perform a pregnancy test – you will need to give a urine specimen for this. Your procedure will be cancelled if there is a possibility that you might be pregnant.
- We recommend you bring a friend or relative with you. Y our clinician may ask them to leave the room depending on the treatment you are having.
Your clinician will also explain the procedure to you and ask you:
- When your last period was
- If you have any allergies
- Whether you have had any reactions to any drugs or tests in the past.
What are the risks associated with a hysteroscopy?
There are risks associated with any procedure. Your clinician will explain these risks to you before you sign the consent form. Please ask questions if you are uncertain.
The most common risks or complications from this procedure include:
- Infection
- A perforation (hole) in your uterus – this is not common, but if it occurs you may need an operation to repair the uterus
- Damage to your cervix – this is not common
- Difficulty seeing the cavity of the uterus
- Heavy vaginal bleeding
- You might feel lightheaded during and after the procedure and may need to rest for the remainder of the day
Patients taking anticoagulant therapy eg Warfarin
Please ensure you have had an INR blood test at least 1 week before the hysteroscopy appointment. The INR level needs to be 2.5 and below prior to the hysteroscopy appointment. If above this level please contact your GP and inform the hysteroscopy secretary as your appointment will need to be rescheduled until the level is correct. Do not stop taking your medication.
Giving my consent (permission)
We want to involve you in decisions about your care and treatment. If you decide to go ahead, you will be asked to sign a consent form. This states that you agree to have the treatment and you understand what it involves.
In some cases, once a diagnosis has been made, the hysteroscope can also be used in the treatment of the problem. For example, problems that can be treated during a hysteroscopy are:
- Fibroids (growths in the uterus which are not cancer)
- Polyps (blood-filled growths which are not cancer)
- Thickening of the lining of the uterus (the endometrium)
- Removal of displaced intrauterine contraceptive devices
- Removal of scar tissue
Are there any alternative treatments?
An ultrasound can also be performed to look at the uterus, but it does not provide as detailed information as the hysteroscopy.
Your Clinician will discuss any alternative treatments with you if you are considering this procedure as a treatment option, for example for fibroids.
What happens during the procedure?
You will have this procedure in the outpatient hysteroscopy clinic you do not need a general anaesthetic, but we may give you a local anaesthetic into the cervix (neck of the womb). Most women do not need this but you can discuss this with your clinician before the procedure. During the procedure a health care assistant will be there to support you. You will be positioned on the gynaecology couch making sure you are comfort and your dignity is maintained at all times.
An instrument, called a speculum, is placed within your vagina to help the clinician see your cervix (the neck of the uterus). A speculum is the same instrument used during a cervical smear. Your cervix may then be opened slightly using a smooth instrument called a dilator local anaesthetic may be used at this point to reduce discomfort. Or alternatively vaginoscopy is performed and a speculum is not required prior to the hysteroscopy.
The hysteroscope (a small, fibre-optic ‘telescope’, which is attached to a small camera) is passed along your vagina and through your cervix in order to look at the inside of your uterus. Sterile fluid is then run into your uterus to expand it – this helps the clinician to see the lining of your uterus.
After the lining of your uterus has been examined, a tiny sample of the lining may be removed. This is called a biopsy.
Small polyps can be removed at this stage using a polyp forcep. The tissue from the biopsies are sent to the laboratory to be examined.
How long does it take and will it be painful?
The procedure takes between 10 and 20 minutes you should plan to be in the clinic for about one hour.
If you are having the hysteroscopy in the outpatient department you will be awake during the procedure. Please do not hesitate to tell the clinician if you feel any discomfort.
Having a General Anaesthetic patient choice
A general anaesthetic may be used because:
- You have expressed that you would prefer to be asleep during the procedure (the benefits and risks of this would be discussed with your clinician)
- Treating fibroids/polyps or the removal of the endometrium can be painful
- It has been decided that another procedure which needs a general anaesthetic, such as a laparoscopy (a procedure which examines the inside of your abdomen) will be done at the same time.
What happens after the procedure?
In the outpatient department:
You might like to arrange for someone else to come to the appointment with you and accompany you home. You should be able to return to normal activities later that day or the next day.
You might feel some period-like pain or cramps. Some discomfort is to be expected during and after the procedure, you can take pain relief (such as Paracetamol) as instructed. If you find that the pain is hard to control, please contact your GP.
What should I look out for at home?
- Vaginal bleeding and discharge
- You might bleed from your vagina for 3 to 4 days following this procedure. This bleeding might be heavier and can stop and start – these variations are normal.
- Please contact your GP if you experience heavy bleeding (soaking a pad every one or two hours) or if you pass any clots larger than the size of a ten pence piece.
- It is normal to have vaginal discharge for up to two weeks after the procedure. Please contact your GP if this discharge becomes offensive smelling, as this might be a sign of an infection.
When can I return to work?
You will be able to return to work the next day however if the bleeding is heavy and you are concerned please see your GP
When can I have sexual intercourse?
Please do not have sexual intercourse for at least seven days after the procedure to help prevent an infection in the uterus or vagina.
When can I use tampons again?
Please do not use tampons during this episode of bleeding. Y ou can start to use tampons again after your next period. This will help to prevent infection.
When can I have a bath or shower?
You can have a shower the day of the procedure and a bath the next day.
Can I eat and drink as normal?
You can eat and drink as normal/
Are there any follow-up appointments?
You might need a follow-up appointment in the outpatient clinic gynaecology department your clinician will inform you.
When will I get the results?
Before you go home, the clinician will talk to you about the findings of the procedure and will write to you and your GP with the results and whether further treatment is needed.
Information about your procedure will be sent by post to your GP
What should I do if I have a problem or concern?
If you have any concerns, please:
- Contact or visit your GP
- Call NHS 111 and speak to a specially trained nurse
- Go to your nearest A&E department or call 999 in the event of an emergency
Contact us
If you have a question about your appointment please contact the Hysteroscopy Patient Pathway Coordinator on 01908 996318 (Internal Calls Ext: 86318)
(Monday to Friday 08.00am to 15.30pm) or the Gynaecology Hub on Ext:
86303 (Monday – Friday 9-5pm)
If you have a query or concerns regarding your hysteroscopy appointment, please contact:
Useful Contacts
Patient Advice and Liaison Service (PALS)
To make comments or raise concerns about the Trust’s services, please contact PALS. Ask a member of staff to direct you to the PALS office at 01908 243633 email: [email protected]
Tell us about your care – The NHS Friends and Family questionnaire Outpatient & Day Patients your comments may be anonymously shared (including online) to help others get great care. iWant great care is an independent organisation allowing patients to provide feedback on their healthcare www.iwantgreatcare.org http://mkhospital.iwgc.net
For more information leaflets on conditions, procedures, treatments and services offered visit our hospital website www.mkhospital.nhs.uk
Language Support Services
If you need an interpreter or information about your care in a different language or format,
020 7188 8815 fax: 020 7188 5953.
NHS 111
Offers medical help and advice from fully trained advisers supported by experienced nurses and paramedics. Available over the phone 24 hours a day.
NHS Choices
Provides online information and guidance on all aspects of health and healthcare, to help you make choices about your health www.nhs.uk