Oesophageal Dilatation Procedure
Please note, this page is printable by selecting the normal print options on your computer.
The oesophagus, or gullet, is the tube that takes food down from the mouth to the stomach. If it becomes narrowed or blocked, there will be a problem with swallowing.
This procedure requires your formal consent. This booklet has been written to enable you to make an informed decision in relation to agreeing to the investigation and treatment. You will be required to sign a consent form on the day of the procedure, which is a legal document, therefore please read this booklet carefully.
If you are unable to keep your appointment, please notify the endoscopy unit as soon as possible. This will enable staff to give your appointment to someone else and to re-arrange another date and time for you.
You need to understand all the information, including the possibility of complications. There will be the opportunity to speak to a healthcare professional about anything that you do not understand on the day of the procedure before you sign the consent form.
What is an Oesophageal dilatation?
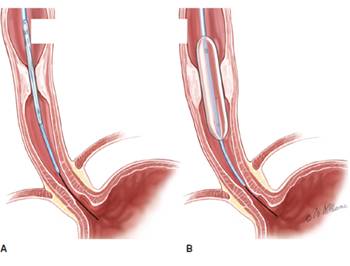
Oesophageal dilatation is a procedure that widens a narrowing in your oesophagus using a special catheter (long, thin tube) with a balloon attached. Dilatation should stretch the narrowing and make it easier for you to swallow. More than one dilatation may be needed over several appointments depending on how much stretching your oesophagus is required.
Are there any alternatives to having an Oesophageal dilatation?
The aim of the dilatation is to allow you to swallow more easily again. There is no alternative procedure that can be done to stretch the oesophagus to allow you to swallow better. If you decided against having this procedure and you can no longer swallow the nutrition the normal way; there are alternatives available, but these are not appropriate for everybody. You’ll need to discuss these with your consultant.
How do I prepare?
To get a clear view of the oesophagus and stomach it is important that the stomach is empty. Please do not eat or drink anything for at least 6 hours before the procedure.
What about my medication?
Routine Medication: If you are on any medication, especially blood pressure tablets, you should take these with a sip of water as usual.
Diabetes: If you have diabetes and control this with insulin or tablets, please ensure that the Endoscopy Unit is aware so that your procedure can be booked for the beginning of the list. You will need to stop your diabetes medication during your “Nil by Mouth” phase. Your usual medication can be recommenced after the procedure once you are eating again. You may want to bring a sandwich with you to eat after the procedure with your usual diabetes medication.
If you have any further concerns, please contact your diabetic specialist nurse well in advance of the procedure for advice.
Anticoagulants/ Antiplatelets: If you are taking blood- thinning medicines, such as Warfarin, Dabigatran, Heparin, Dalteparin, Apixaban Clopidogrel, the dose of these may need to be altered or stopped before your procedure. You may also need to have blood tests before your procedure. If the referring doctor did not give you instructions, you may be referred to the bridging clinic for advice on stopping your medication. If this is required, this will be arranged for you by the referring clinician or the endoscopy booking coordinator.
What to bring with you?
Along with your appointment letter you will have received a health questionnaire. Please complete it and bring it with you. You will also find enclosed a copy of your consent form; please read this carefully but do not sign it. This is just an example for you to read carefully prior to your appointment. The endoscopist will meet with you prior to your endoscopy to discuss what is going to happen, any risks and any serious or common side effects. At this point you will be given the opportunity to ask any questions and then you will sign the ‘actual’ consent form.
How long will I be in the Endoscopy unit?
You should expect to be in the unit for approximately 5 hours. Please note that the time of your appointment is not the time that the procedure will be performed. How long you will be in the unit will depend on how quickly you recover from the procedure, the sedation you may have had and also on how busy the unit is. The unit also looks after emergencies, and these can sometimes take priority over outpatient procedures.
You should be kept informed of any delays, but if you have any questions or concerns, please ask a member of the staff.
What will happen when I arrive?
After checking in at reception, a qualified nurse will welcome you and take you to the admissions area where you will have a brief medical assessment. Please note that the endoscopy unit operates a same sex environment and your relative may not be able to accompany you past the waiting area unless there are exceptional circumstances. In the admission room, you will be asked some questions regarding your medical and surgical history to confirm that you are fit to undergo the procedure and about your arrangements for getting home. The nurse will make sure that you understand the procedure and discuss any questions you may have.
Your blood pressure, heart rate, respiration and oxygen levels will be recorded. If you have diabetes, your blood sugar level will also be checked and recorded.
If you wear spectacles or dentures you will be asked to remove them when you enter the procedure room. All your belongings will be kept with you during your procedure to prevent anything being lost. You are advised to leave your valuables at home as we do not accept responsibility for them.
Many people decide to have a gastroscopy just with a local anaesthetic throat spray to make the throat numb. However, some need a little bit more help to keep them relaxed. If you have decided that you want sedation, which will be given later, the nurse will insert a cannula (a small plastic tube) into a vein in your hand or arm.
Sedation
Usually, an intravenous sedation is offered for this procedure, you can discuss this with the endoscopist before the procedure. A sedative (usually Midazolam) and/or a painkiller (Fentanyl or Pethidine) may be offered which will be administered through an IV cannula (a plastic tube) which is inserted in a vein in your arm/hand. This will make you slightly drowsy and relaxed, but not make you go to sleep like a general anaesthetic. You will still hear what is said to you and therefore, will be able to carry out simple instructions during the procedure. Some people do not remember anything about the procedure once the effects have worn off.
Whilst you are sedated, we will monitor your breathing, respiration, and pulse rate via a finger probe, so that any changes can be recorded and dealt with accordingly. You will also be given some oxygen via a nasal sponge into your nostril. Your blood pressure may also be checked and recorded.
If you are having sedation, you must arrange for a responsible adult to collect you and stay with you overnight. If you have not been able to make these arrangements, you will not be able to have the procedure with sedation. You should not drive, return to work, operate machinery, or drink alcohol for 24 hours after the procedure, nor should you make any important decisions. The reason for this is that the sedation may, even though you may feel perfectly normal, still be in the body and may impair your judgement.
The procedure
After signing your consent form in the admission area, you will be escorted to the procedure room, you will be introduced to the team and a verbal safety checklist (called “WHO”) will be done. Your throat will be made numb by using the local anaesthetic spray; you will then be asked to lie on your left side. A “probe” will be placed on your finger which can read your pulse and the amount of oxygen in your body (pulse oximeter). Oxygen will be given, usually via a sponge which is placed into one of your nostrils. A mouth guard is placed lightly between your teeth.
The Doctor passes a flexible tube (endoscope) down through your throat, into your gullet and assess the narrow area. A balloon catheter is then passed down the narrow area. When the balloon is in the correct position, it is expanded to stretch the narrowing. This may be repeated several times. During this time X-ray may be required as it minimise the risk of complications.
Once the doctor is happy with the dilatation; the endoscope is then gently passed across the dilated area to examine the stomach and duodenum. The procedure should take about 20 minutes.
Will it hurt?
Sometimes, during the procedure, people may experience chest or back discomfort/ pain, this usually settles within a couple of days. Please let your nurse and/or doctor know if you do have discomfort or pain as pain relief medication can be given to help you feel more comfortable.
Aftercare
After your procedure you might need to have a chest x-ray to check. Your nurse will tell you when you are allowed to have a drink and something soft to eat. This may be a few hours. Before you go home the Dietitian and/or your key worker (your Upper Gastro-Intestinal (UGI) Nurse Specialist) may come and talk to you about types of food you can have. This is mainly about having plenty of fluids to drink, particularly with your meals. Please be aware that there will be some types of food that you will still need to avoid.
Here are some simple tips:
- Sit upright to eat.
- Take small mouthfuls of food.
- Eat slowly and chew your food well.
- Use plenty of sauces, gravy and butter to moisten food.
- If your appetite is poor, consider having smaller and more frequent nourishing meals.
Are there any risks or complications?
Having an Oesophageal dilatation does have some risks associated with it. These occur infrequently, but we wish to draw your attention to them to help you make your decision. The doctor or specialist nurse who has requested the test will have considered this already. The risks must be compared with to the benefit of having the procedure carried out. The risks can be associated with the procedure itself and the administration of the sedation.
Complications can happen. The possible complications are listed below. Any numbers which relate to risk are from studies of this procedure. Your doctor will tell you if the risk of complications is higher or lower for you.
- Sore throat, which gets better quickly.
- Allergic reaction to equipment, materials, or sedative. The endoscopy team is trained to detect and treat any reaction that may happen. Let the admitting nurse and endoscopist know if you have any allergies or you have reacted to any drugs or tests in the past.
- Breathing difficulties or heart irregularities, as a result of reaction to sedation or inhaling secretions such as saliva. To help prevent this from happening, your respiration and oxygen levels will be monitored, and a suction device will be used to clear any secretions. Rarely, a heart attack or stroke (loss of brain function resulting from an interruption of the blood supply to the brain) can happen if you have serious medical problems.
- Perforation – making a hole in the oesophagus (risk: 1 in 300). If a hole occurs, you will need to be admitted to hospital for further treatment. If it is a small hole, it can heal with rest from feeding and antibiotic. Larger holes may require surgery to repair them.
- Damage to teeth and bridgework. The nurse will place a plastic mouthpiece in your mouth to help protect your teeth. Let the endoscopist and nurse know if you have any loose teeth.
- Bleeding from the treated are or from minor damaged caused by the dilatation. This usually stops on its own.
- There is slightly increased risk of developing chest infection after this procedure.
- Incomplete procedure. This can happen due to a technical difficulty, food or blockage in the upper digestive system, complications during the procedure, or discomfort. Your doctor may recommend another endoscopy or a different test such as barium meal.
- This can occasionally cause problems with breathing, heart rate and blood pressure. If these problems do occur, they are usually short lived. Careful monitoring by the endoscopy team ensures that any potential problems can be identified and treated quickly. Older patients and those with significant health problems such as breathing difficulties due to a bad chest may be assessed by a doctor or specialist nurse before having the procedure.
- Complications can happen. Some of these can be serious and can even cause death (risk: 1 in 25,000).
You should discuss these possible complications with your doctor if there is anything you do not understand.
What to do if you feel unwell once you’re home
If you have persistent abdominal or chest pain, fever, or bleeding after the procedure, you must then seek urgent advice from the Endoscopy Department between 09:00 and 17:30 (01908 996 460) Monday to Saturday.
Outside these hours, please call a nurse on Ward 22 (01908 996 455) for advice or go to your nearest A&E department.
