Nephrotic Syndrome
Please note, this page is printable by selecting the normal print options on your computer.
About the Urinary System
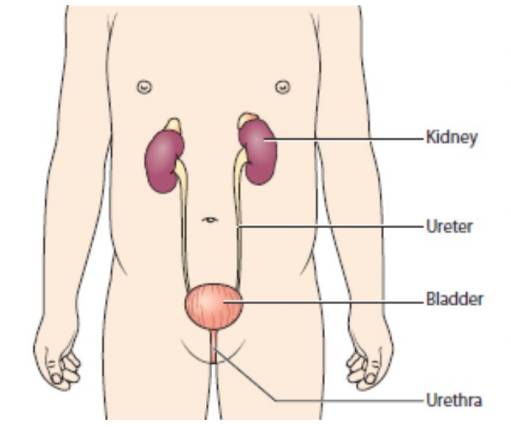
The urinary system gets rid of things that the body no longer needs, so that we can grow and stay healthy. The kidneys are bean-shaped organs. They filter blood and remove extra water and waste in urine (wee). Normally there are two kidneys. They are at the back on either side of our spine (backbone), near the bottom edge of our ribs.
The two ureters are long tubes that carry urine from the kidneys to the bladder. The bladder is a bag that stores urine until we are ready to urinate (wee). It sits low down in the pelvis. The urethra is a tube that carries urine from the bladder to the outside of the body. We urinate through the opening at the end of the urethra.
What is Childhood Nephrotic Syndrome?
In nephrotic syndrome, the kidneys leak too much protein into urine, leading to a drop in the levels of protein in the blood. This causes swelling in the body, especially in the face, legs and feet.
About nine in ten children with nephrotic syndrome have a type that can be treated with a steroid medicine. This is steroid-sensitive nephrotic syndrome (SSNS), because it is “sensitive” to steroids. It is sometimes called minimal change nephrotic syndrome (MCNS) or minimal change disease.
Symptoms and Complications
The main symptom of nephrotic syndrome is swelling in the body – this is called oedema. In children, the swelling is mainly around the eyes and in the legs and feet. The swelling happens because the kidneys leak a lot of protein in the urine (which is called proteinuria). You cannot usually see the protein, though it can be found in a simple urine test.
Tests and Diagnosis
Your doctor can diagnose (identify) nephrotic syndrome by doing a physical examination, asking about the symptoms and doing a urine test to look for protein. Your child may need other tests, such as blood tests.
Treatment
Your child will probably need to be admitted to hospital for a few days or longer. He or she will need to take a steroid medicine – usually prednisolone. Most children start to get better after taking steroids for 1 to 2 weeks. In about 9 in 10 children, the nephrotic syndrome will have responded to the steroids within 4 weeks. Some children need to take other medicines to help prevent or treat infections or to reduce the oedema (swelling).
Monitoring
You will need to test your child’s urine for protein every morning – while your child is on steroids, and then for at least 6 months. A nurse will show you how to do this. If there is no or very little protein in the urine and the swelling goes down, the nephrotic syndrome has gone into remission. If there is protein in the urine again, this is a relapse. You will need to contact your doctor, and
your child may need another course of steroid medicines.
Caring for your Child at Home
If your child has been diagnosed with nephrotic syndrome, you’ll need to monitor their condition on a daily basis to check for signs of relapses. You’ll need to use a dipstick to test your child’s
urine for protein the first time they urinate each day. The results of a dipstick test are recorded as either:
• negative
• trace
• 1+
• 2+
• 3+
• 4+
The result for each day needs to be written down in a diary for your doctor or specialist nurse to review during your outpatient appointments. You should also note down the dose of any medication they’re taking and any other comments, such as whether your child’s feeling unwell. If the dipstick shows 3+ or more of protein in the urine for 3 days in a row, this means your child is
having a relapse. If this happens, you either need to follow the advice given about starting steroids or contact your doctor.
You should seek immediate medical advice if:
• your child has come into contact with someone who has chickenpox or measles and your doctor has told you that your child is not immune to these illnesses
• your child is unwell or has a fever
• your child has diarrhoea and is vomiting
About the Future
Relapses
About half of children with SSNS will have at least one relapse, and many have two or three relapses. In most children, the SSNS tends to relapse less often as they grow into their teenage years. It is rare that SSNS continues to relapse in adulthood. If your child’s nephrotic syndrome keeps coming back, this is called frequently relapsing nephrotic syndrome. Your doctor will consider the best treatment for your child.
Follow up
Your child may be allocated a Children’s Community nurse on discharge, who will monitor your child’s blood pressure and urine tests. All children with nephrotic syndrome need to go back to the hospital or clinic for follow-up appointments to check for any health problems. Remember to bring the results from your urine testing.
If you have any concerns you are welcome to contact the Paediatric Community nurses on 01908 996518 Monday-Friday 9-5 or Paediatric Assessment Unit on 01908 996368.
Kidney problems
A very small number of children with nephrotic syndrome have more serious problems with their kidneys. Your doctor will refer your child to a paediatric nephrologist, a children’s kidney doctor,
for more specialist treatment.
Additional Information and Support is Available via:
www.infoKID.org.uk
Resources Used:
Kidney Care UK
Royal College of Paediatrics and Child Health
NHS Choices
