Neck dissection information
Please note, this page is printable by selecting the normal print options on your computer.
This has been written as a guide for anyone having surgery to remove the lymph glands in their neck. It has been compiled by experienced staff and answers the questions most frequently asked by patients.
This information is only a guide and your healthcare team will give you more detailed information as you need and want it.
How do cancers spread?
Most cancers which start in the head and neck region have the ability to spread to other parts of the body; these are called metastases or ‘secondaries’.
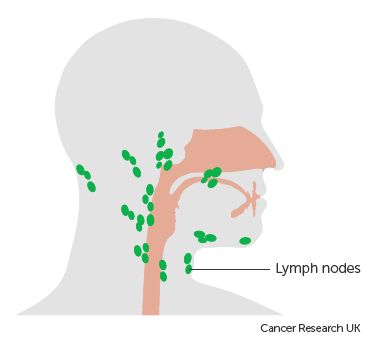
Cancers can spread in different ways. In the head and neck region lymphatic spread to the neck is fairly common. Sometimes cancers can spread throughout the lymphatic system to distant areas of the body. Lymph nodes or “glands” are like sieves, which catch any bacteria, viruses or cancer cells in the body. The nodes in the neck drain the skin of the head and neck and all the swallowing and breathing tubes.
Once one cancer cell has been ‘caught’ by a lymph node it can grow and multiply there and, in time, can spread to the next node down the chain and so on. Lymph node removal is carried out by an operation called a neck dissection.
What is a neck dissection?
There are different types of neck dissection, each used for different reasons. Your surgeon will discuss with you the details of the operation you are having.
Radical neck dissection
A radical neck dissection is a surgical operation which aims to remove all the lymph nodes in the neck between the jaw and the collarbones. This is usually planned if there is evidence that several lymph nodes in the neck are affected and particularly if they are bulky. Because the nodes are small and stuck to other structures in the neck, they are usually removed with some surrounding tissues as well, to make sure all the diseased tissue is removed. The only structures which are removed are those which you can safely do without.
Selective neck dissection
A selective neck dissection is performed in the majority of cases when the amount of disease in the neck is small or when there is a suspicion that there may be microscopic amounts of cancer cells in your neck. In this case, only the groups of lymph nodes that experience has shown to be most often affected in your type of cancer are removed. In both operations the tissues are sent to the laboratory to search for cancer cells and to see how extensive the spread has been.
What can I expect from the operation?
In many cases the neck dissection is only part of the whole operation you will be having; often there is a need to remove the primary tumour.
The operation is performed under general anaesthesia, which means that you will be asleep throughout. The surgeon will make one or two long cuts in the neck. The skin is then folded back to allow access to the underlying structures.
After the operation
At the end of the operation you will have 1 or 2 drain tubes coming out through the skin, as well as stitches or skin clips to close the wounds. You will be advised when these need to be removed (this is usually by the practice nurse at your GP surgery).
The scars usually run along the natural creases of your neck. When the skin is lifted up during the operation it loses its nerve supply and so may be numb after the operation. This means that most people do not have much pain afterwards, but if you do have pain, this can be well controlled with pain killers, which you will be offered.
If removal of one of the large muscles from the neck is necessary, the neck will look a little flatter on the side of the surgery. You will probably feel quite drowsy for most of the day, following a general anaesthetic. If your neck dissection forms part of a more major operation, you may spend 1-2 days in the intensive care or high dependency unit (at Northampton General Hospital), before being transferred to the head and neck ward.
For Milton Keynes patients, if your surgery is on a Thursday or Friday, there may be the need to transfer you to Northampton General Hospital for ongoing care from the head and neck team (a leaflet will be provided to you by the ward explaining this).
What is the risk of complications and side effects?
- Numb skin – As mentioned above, the skin of the neck will be numb after the surgery. This will improve to some extent, but you should not expect it to return to normal.
- Stiff neck – You may find that your neck is stiffer after the operation. You may require further physiotherapy for your neck and shoulder if they are affected.
- Haematoma – Sometimes the drain tubes which are put in at surgery block, or fail to work, in which case blood can collect under the skin and form a clot (haematoma). If this happens, further surgery may be required to remove the clot and replace the drains.
- Chyle leak (pronounced ‘kile’) – Chyle is the name given to digested fats that are carried from the gut in the lymphatic system. Occasionally one of the lymph channels, called the thoracic duct, is damaged during a neck dissection, usually on the left side. This can be hard to spot during the operation. If this occurs, chyle can collect under your skin or may be seen in your neck drain.If you have a chyle leak you will usually be placed on a fat-free or modified fat diet for a period of time (usually 2-3 weeks) until the leak has healed, or you may be taken back to theatre to repair the leak. Very occasionally, it is necessary to feed you intravenously. We would therefore need to keep you in hospital longer than originally planned.
- Damage to the accessory nerve – This is the nerve to one of the muscles of the shoulder. Surgeons try hard to preserve this nerve but sometimes it needs to be removed because it is too close to the tumour to leave behind. In this case you will find that your shoulder is a little stiff and that it can be difficult to lift your arm above the shoulder. Also lifting heavy weights, like shopping bags, can be difficult.Even if the nerve is preserved, it may sometimes be bruised by the surgery. Innervation issues are very individual and some people may not notice any difference to the function of the shoulder. Again, further physiotherapy may help to maximise your shoulder movement.
- Damage to the hypoglossal nerve (nerve that moves the tongue) – Very rarely removed unless involved with the tumour, but if it is, you may not notice any obvious changes. If there is any significant functional changes, speech and language therapy can be provided.
- Marginal mandibular nerve damage – This nerve is also at risk during the operation, but surgeons try hard to preserve it. If it is damaged you will find that the corner of your mouth will be a little weak. This is most obvious when smiling. Lip closure may be weaker on that side, which may occasionally result in a little dribbling when eating and drinking. The speech and language therapist can suggest exercises and strategies that may help improve this function.
- Lymphoedema – After surgery to remove lymph nodes from the neck, you can develop long-term swelling. This happens because the lymphatic system, which normally drains fluid away, isn’t working properly. It may be worse in the morning and improve as the day goes on. As well as causing swelling you can see in the face or neck, it can also affect tissues inside the neck, such as the throat or larynx (voicebox). This can cause difficulty speaking, swallowing or breathing. Lymphoedema is usually treated by a lymphoedema therapist. Your GP, specialist doctor or health professional at the hospital can refer you to one.
When will I be admitted for surgery?
You will be asked to attend an appointment in the pre-assessment clinic before surgery. During this appointment we will assess your fitness to undergo a major operation.
You will be admitted via the Same Day Admissions Unit (SDAU) on the morning of your surgery, or the afternoon, before if the neck dissection is part of more major surgery (at Northampton General Hospital).
Admission time will also vary if you have other medical conditions that require earlier admission. You are likely to stay in hospital between 3-7 days, depending on the extent of the operation. Your surgeon should be able to give you an estimate of the total length of stay.
Will I need any other sort of treatment?
This will depend very much on what treatment you have already had, where your tumour is and what type of tumour it is. Sometimes you may also need to have radiotherapy to improve your chance of a cure. This will be discussed at your first post-operative outpatient appointment.
If you have any questions or concerns, or need any further information, please contact us. You should already have been given contact details of your nurse specialist or key worker, so that is usually the best place to start.
Helpful Contact Numbers
Head and Neck ANP 01908 996 794
Mr. P. Gurr – Secretary 01908 995 264
Speech and Language Therapy 01908 725 299
Milton Keynes University Hospital 01908 660033
Ward 23 01908 995 473
ENT Outpatient 01908 995 366
