Laparoscopic Cholecystectomy
Please note, this page is printable by selecting the normal print options on your computer.
Laparoscopic Cholecystectomy
Gallstones have been found in your gallbladder. These may have caused you pain and/or other symptoms. Your doctor has recommended an operation called a Laparoscopic Cholecystectomy to treat your symptoms. Laparoscopic is the medical term for keyhole surgery, Cholecystectomy is the medical term for the removal of the gallbladder. Therefore, a Laparoscopic Cholecystectomy is the removal of the gallbladder using keyhole surgery.
What is the gallbladder?
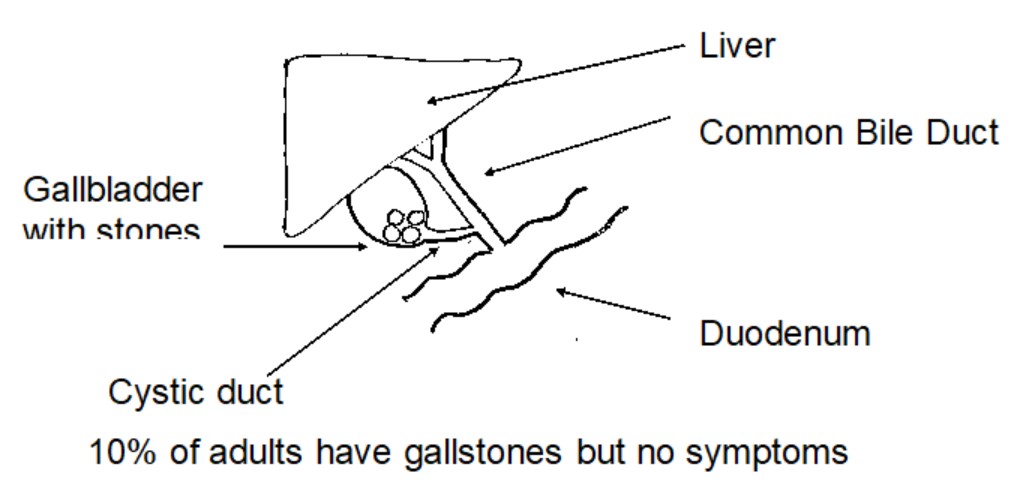
The gallbladder sits just under the liver and is found in the right upper right part of the abdomen, just under the ribs and acts as a reservoir for bile. It is attached to the side of the bile duct where bile can be stored and concentrated between meals. Bile is a green liquid made by the liver that drains from the liver to the intestine via the bile duct. When we eat, particularly fatty foods, the gallbladder contracts and empties extra bile into the bile duct and then into the intestine to mix with the food. Bile has many functions, one of which is to allow us to absorb fat.
Why do I need my gallbladder removing?
- Sometimes your gallstones cause inflammation of the gallbladder and this is called acute cholecystitis. This needs treatment in hospital with antibiotics. Occasionally, the stones may cause obstruction and lead to jaundice.
- If you have gallstones you may have experienced pain, nausea and vomiting after eating food. This is called biliary colic and is because the gallstones are moving within the gallbladder and the cystic duct (which is the pipe out of the gallbladder).
A ‘fat free’ diet whilst awaiting surgery may help to alleviate symptoms and pain.
What are the alternatives to a Cholecystectomy?
Other treatments have been tried, but have not been very successful – they fail to eliminate the stones completely and new stones form. Drugs are available to dissolve some gallstones, but they do not dissolve all gallstones and it is impossible to tell which ones will dissolve without removing some. The drug treatments have many side effects and the gallstones recur once the drugs have been stopped. These are not widely used in Britain.
The only way to remove the stones permanently is to have an operation that removes the gallbladder. Removal of the gallbladder is not associated with any impairment of digestion in most people.
What is ERCP?
Some patients require the telescopic procedure ‘Endoscopic Retrograde Cholangiopancreatogram (ERCP)’. This involves being sedated and then putting a telescope through your mouth, through to your stomach. Some dye is then injected into the pipe that drains your liver (the common bile duct) and if there are any stones in your common bile duct they can be removed. If you have been jaundiced you will need an ERCP.
If you have the ERCP it may be recommended that you still need your gallbladder removing. This is because the gallbladder can still produce and may still contain gallstones, which could continue to cause problems.
Pre-Assessment
All patients who are coming for elective Laparoscopic Cholecystectomy will attend for a pre-assessment. This assessment will allow the nurse to provide a full health screen. This helps us to know that you are fit for an anaesthetic and your operation. Our main aim is to minimise the chance of your procedure being cancelled on the day of surgery.
Day of Surgery
Please follow the instructions that you are given. You must not eat or drink anything or chew chewing gum before your operation. This is to make sure your stomach is empty, as it is dangerous for you to have an anaesthetic if your stomach is full. If you do not follow these instructions, your operation will be cancelled.
An anaesthetist (the Doctor who looks after you when you are asleep) will come to the ward to ask some questions.
You will also be seen by a member of the surgical team who will want to ask you some questions and will obtain your consent for your operation. It is normal for you to consent to ‘Laparoscopic Cholecystectomy +/- open’ – this means you are consenting have the keyhole procedure, but if necessary, you have consented to an open operation should the surgeon require to do so when you are under a general anaesthetic.
One of the ward nurses will also ask you some questions.
There will be many patients admitted for surgery and some waiting is to be expected. Before proceeding to theatre, a checklist will be performed and you will be asked to remove all jewellery, dentures, contact lenses, makeup and change into your gown.
When it is time for your operation you will be taken to the theatre department where a member of the theatre team will meet you. You will be asked similar questions to those you were asked on the ward, these are routine checks for your own safety. After this you will be taken into the Anaesthetic room where some monitoring equipment will be attached to you. At this time the anaesthetic will be given to you.
What does the operation involve?
This is an operation involving a general anaesthetic (going to sleep). Three to four small holes (about ½ cm to 1cm long each) are made in the tummy wall. Through these, special long instruments are used to free up the gallbladder with its stones from underneath the liver and it is completely removed. This is all visualised on a TV screen by a miniature camera that is inserted through one of the four keyholes. In addition, it is sometimes necessary to perform an X-ray during the operation called a Cholangiogram. This is used to check for stones in the bile duct.
What are the benefits of Laparoscopic Surgery?
Using the keyhole method will cause you to suffer less pain and may allow you to return home on the same day, or after only a short stay in hospital. During the surgery, if it is particularly difficult or there are problems with bleeding, or it is unsafe to proceed with keyhole surgery, the surgeon will make a decision to perform an Open Cholecystectomy. This involves a larger cut in the abdomen and may require you to stay in hospital for up to 5-6 days.
Are there any reasons why I could not have Laparoscopic Surgery?
If you had surgery in the area of your gallbladder before, if you tend to bleed a lot, or if you have any problems that would make it hard for your doctor to see your gallbladder, an open surgery may be better for you. Your surgical team will discuss which type of surgery is appropriate for you.
After the Surgery
Following surgery you will be taken to the recovery room where you will be monitored before returning to the ward. You will have some discomfort from the scars and occasionally the gas in the abdomen that is left after the operation can cause discomfort or pain in the shoulders. This may continue for a few days. You may also feel nauseated, but this will pass.
If you have any pain or nausea (feelings of sickness), please let the nurses know. Pain relief is important, not only for your comfort, but also to allow you to move around in bed, breathe deeply and cough. This is vital if you are to avoid problems of chest infections.
You may have a drip (to give you fluid while you are not drinking or eating normally). You will be able to drink, take sips to begin with and then build up. The nursing staff will be able to advise you when you can take diet. You may have a drain inserted and this will be removed prior to going home.
When you are discharged the nursing staff will advise you about your follow up appointment and if you have any stitches in your wounds that are not absorbable and that require to be removed. The nursing staff will provide a letter for you and one for your doctor. Discuss with the nursing staff what painkillers you have at home. It is advisable to wear loose fitting clothes as your abdomen may be slightly distended due to the gases for the procedure.
What are the risks?
Surgery is usually very safe and effective. However, risks and complications can occur. You need to be aware of them in order to make an informed decision about surgery. Knowing about them will also help with early detection of a problem and help with early treatment. If you are worried about anything, whether in hospital or at home, ask a member of the healthcare team. They should be able to reassure you or identify and treat any complications.
General complications of any operation.
- Pain – occurs with every operation. Efforts will be made to minimise the pain. A local anaesthetic may be injected into the skin to ease the pain for several hours after the operation. You will be given medication to control the pain and it is important that you take it as instructed so you can move about and cough freely.
- Bleeding – can occur either during or after the operation. This rarely needs a blood transfusion or another operation, but it is common to get bruising of the abdomen. This can be marked and cause a swelling around the wound, but normally settles in a week or two.
- Infection – in the surgical wound, which needs treatment with antibiotics. This usually settles after a few days.
- Scars – a small percentage of people have an inherited tendency to scars that are unusually red and raised. This may cause an unsightly scar, but is of no further consequence.
- Blood clots – in the legs (thrombosis), which can occasionally move through the bloodstream to the lungs, causing breathing difficulties (emolus). You will be encouraged to get out of bed soon after the operation. Most people are given compression stockings to wear during the operation, though some are also given an injection in the skin to thin the blood.
Complications of any Laparoscopic Surgery
- Damage to internal organs – when placing instruments into the abdomen. This is rare (Risk 1 in 2,000). The risk is higher in patients who have previously had surgery to the abdomen. If an injury does occur, open surgery may be needed. About 1 in 3 of these injuries are not apparent until after surgery, so if you have pain, which does not improve two days after surgery, you must let your doctor know.
- Surgical emphysema – (Crackling sensation in the skin due to trapped gas) which settles quickly and is not serious.
- If there are unexpected difficulties with the operation, then it may be necessary to open your abdomen in the conventional way. This happens in about 5% of operations. Reasons for this could include scarring internally from other operations (adhesions, bleeding or injury to the bowel or common bile duct), which are in close proximity to the gallbladder.
- In up to 1% of cases bile can leak into the abdomen after the surgery. Bile is very irritant and causes pain and tenderness. In this situation it may be necessary to undergo a procedure to washout the bile and insert a temporary drain. This can sometimes be done under local anaesthetic by one of the radiologists but on other occasions will
- require a general anaesthetic and a further keyhole surgery procedure. If the leak is persistent an ERCP may be required. Once the leak has settled there are not usually any further problems
- In around 0.5% of people the common bile duct can be damaged and this requires major surgery to rebuild the common bile duct. Sometimes this has to be carried out at another hospital.
- The onset of fever, yellow skin or eyes, worsening abdominal pain, distention, persistent nausea or vomiting, or drainage from the incision are indications that a complication may have occurred. Your doctor should be contacted in these instances.
On discharge – at home
Most patients will be able to go home the same day. However, in a few cases it may be necessary to stay overnight. Your team will discuss this with you.
- It is essential that you have a responsible adult to take you home, either by car or taxi.
- During the first few days you may be tired easily, but this will pass and gentle exercise is beneficial.
- It is normal to have swelling/bruising around your wound and this will settle over a week or two. However, if the area becomes hot to touch, very painful, or you are feverish, please contact your own GP.
- Avoid heavy lifting or strenuous exercise for 1 (one) week.
- Depending upon the nature of your job you may return to work as soon as you are comfortable. This is normally about 2 weeks for a desk job and 4 weeks for a manual job.
- You must not drive for at least 48 hours after your operation due to the effects of the anaesthetic drugs. You can begin to drive when you feel comfortable and confident enough to do an emergency stop safely. It is always best to check with your insurance company over cover as they may have their own guidelines for you to follow.
- You may resume your sex life when you are ready.
- A general anaesthetic remains in your system for 24 – 48 hours. Therefore, it is important to have a responsible adult to care for you following your operation.
- Avoid staying in bed for long periods, gentle exercise is important as soon as you can.
Diet
There are no restrictions to the foods you can eat following gallbladder surgery. For the first few days, you should eat a light diet.
After discharge, if you have any problems, please contact your own GP or non emergency number 111.
References for the information used in this leaflet may be obtained from the author.
People are unique and the alternatives, risks and benefits will of course vary from person to person. We hope this leaflet will support the information you have already received from your doctor in enabling you to make an informed decision.
