Information for adult patients with diabetes undergoing surgery
Please note, this page is printable by selecting the normal print options on your computer.
This leaflet has been designed to give you information about:
- The importance of diabetes management when you are having surgery.
- How to prepare for surgery, including changes to your medication.
- Instructions for the day of surgery.
- Managing your blood sugar on the day of surgery.
- How to manage your diabetes when you go home after surgery.
Before you come into hospital for your operation, please make sure that you have read through this leaflet so that you are fully supported.
The Importance of Diabetes Management and Having Surgery
Introduction
Understanding your diabetes is key as you prepare for surgery. Diabetes is a condition where your blood sugar level is too high, usually because your body does not produce enough insulin, the insulin is not effective, or no insulin is made at all.
Persistently high blood sugar levels can, over time, affect your heart, eyes, feet, and kidneys – these are known as diabetes complications. However, good blood sugar management and diabetes care can help people live healthily and greatly reduce these risks.
Why Does Blood Sugar Management Matter?
Managing your diabetes well is especially important before surgery to support your healing and recovery. You are less likely to have problems like infections after surgery. You are also more likely to heal faster, recover quickly, and have a shorter hospital stay.
How Can We Measure Your Blood Sugar Control?
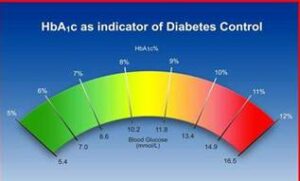
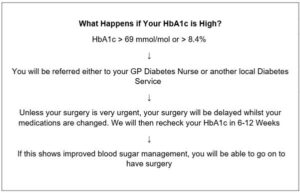
Doctors use a blood test called HbA1c to check your average blood sugar over the past 3 months. Your HbA1c should ideally be 69 mmol/mol or 8.4% or lower before surgery.
Note: HbA1c is different from a regular blood sugar reading, which measures how much sugar is in your blood at a particular moment.
If your HbA1c is too high, it could cause problems during or after surgery. For your safety and to get the best outcome, your surgery might need to be postponed until your HbA1c improves. While a delay can be frustrating, it allows for adjustments to your diabetes care, getting you ready for your procedure.
How to Prepare for Surgery
Changes to Your Diabetes Medication
Before your surgery, you may need to fast for a short period, which means stopping eating or drinking. This can affect your blood sugar, so some diabetes medications might need to be reduced or stopped temporarily. With good planning, these changes should not cause problems with your diabetes management.
Written below are instructions from your pre-assessment nurse. Please make sure you follow these carefully. If your medications are not adjusted correctly, your surgery might be delayed or cancelled for your own safety.
Remember: Following pre-surgery instructions leads to safe and successful surgery
Instructions for changes to your medication prior to surgery (to be entered here by the Pre-assessment Nurse)
| Your Diabetes Medication | Change instruction |
What to Bring to the Hospital
- This leaflet with all your instructions
- Hypo treatments (in case of low blood sugar)
- Blood glucose testing equipment (e.g., blood glucose meter)
- Diabetes medications (pills, insulin, etc.)
- A supply of insulin needles (if you take insulin or other injectable treatments)
Preparation for Surgery Checklist
- Read your pre-surgery information
- Check and follow your medication instructions
- Follow your eating and drinking instructions
- Remember to bring your medications with you
- Prepare for surgery & manage blood sugar
Instructions for the Day of Surgery
Your pre-surgery instructions may vary depending on whether you are having morning or afternoon surgery. Please arrive at the hospital on time. Here is what to expect:
For Morning Surgery
- Arrive at the hospital by 7:15 am.
- Stop eating/drinking:
- No food or drinks (tea, coffee, juice, milk) after 2:30 am.
- You can drink only water after 2:30 am.
- At 6:00 am, drink a glass of water (finish by 6:30 am).
- No sweets or gum: Avoid sucking on sweets or chewing gum.
- Bring all your medications: Bring your medicines in their original containers, including over-the-counter medications, herbal products, and inhalers.
For Afternoon Surgery
- Arrive at the hospital by 11:45 am.
- Light breakfast before 7:30 am: Examples include:
- Two slices of toast or
- A bowl of cereal
- Tea or coffee
- No food after breakfast: You can only drink water after 7:30 am.
- At 11:00 am, drink a glass of water (finish by 11:30 am).
- No sweets or gum: Avoid sucking on sweets or chewing gum.
- Bring all your medications as mentioned above.
Special Instructions for Insulin Users
- If you use insulin, check your blood glucose every 2 hours starting from 6 am on the day of your surgery.
- Record your blood sugar levels and bring the record with you.
- If you are using an insulin pump, tell the staff. Some procedures may interfere with the pump.
-
- For guidance, contact your diabetes team
Managing your blood sugar on the day of surgery
On the day of surgery your blood sugar will be checked. If it needs adjusting, the team will ensure it is stable before going ahead with your procedure
What happens if your blood sugar is high?
If your blood sugar is high (more than 12mmol/L on at least 2 occasions) you will be given treatment to lower it before your surgery. This may include a single dose of insulin which is given by injection under the skin.
Occasionally, when you must fast for a long time or you are unwell, the team looking after you may decide it is best to give you insulin directly into a vein (intravenously) as an infusion. If this is started, your blood sugar will be checked every hour while you are receiving this treatment. This is a temporary treatment, and once you are well enough to eat and drink again, the intravenous insulin will stop, and you will return to your normal diabetes medications.
What happens if your blood sugar is low? (Hypoglycaemia)
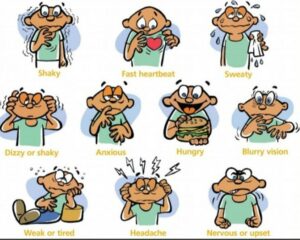
If your blood glucose is too low (below 4 mmol/L), you may experience symptoms like:
- Sweating
- Shaking
- Dizziness
- Blurry vision
- Headache
- Feeling weak or tired
- Feeling anxious, nervous or upset
- Having a fast heartbeat
If you have a low reading, you need to treat it quickly. You will be asked to
- Take fast-acting glucose (15-20g), even if you feel fine.
- Examples: 150-200 ml of clear apple juice or Lift glucose juice.
- Recheck your blood sugar in 10-15 minutes.
- If it is still below 4 mmol/L the treatment will need to be repeated.
Please inform the hospital staff if you have experienced a hypo and have treated it.
What to do if you have questions about your diabetes management while you are in hospital?
If you have any questions or concerns during your hospital stay, please ask to be referred to the Diabetes Inpatient Nursing Team. Visit our webpage for more information about managing diabetes www.mkuh.nhs.uk/diabetes-care. Scan the code below to access the webpage on your device.
After Your Surgery
Once your surgery is finished, you will be offered food and drink when you are ready. Once you can eat and drink normally again, you can start taking your usual diabetes medication again from your next meal onward. Your healthcare team will provide you with more guidance on this.
How to Manage Your Diabetes When You Go Home After Surgery
At Home:
- Continue your usual diabetes medication (whether it is tablets or insulin) as advised by your healthcare team.
- Check your blood sugar if you normally do this or have the necessary equipment. It is good to check up to 4 times per day (before meals and at bedtime).
- Your blood sugar may be higher than usual for a day or two after surgery. This is usually nothing to worry about unless you feel unwell.
- If you feel unwell, especially if you are vomiting and cannot eat or take your medication, contact your usual diabetes team, your GP surgery, or call 111. Be sure to tell them that you have recently had surgery.
Follow-Up on Your Diabetes Care
You will be informed if any follow-up care is needed for your diabetes, either by your surgery team or your Diabetes team. If no follow-up is needed, you should continue to monitor your diabetes and keep attending your regular GP appointments as usual.
Need Help?
If you do not understand the instructions or need help, please ask a member of your diabetes care team, your nurse, or your doctor.
