Information for adult patients with diabetes undergoing surgery
Please note, this page is printable by selecting the normal print options on your computer.
You have been given this leaflet because you have diabetes and are having surgery.
Diabetes control is important, especially around surgery
It has been shown that patients whose diabetes is well managed before their operation are less likely to have complications such as infections after surgery. Blood glucose control can be trickier before an operation as you are required to fast (stop eating or drinking for a short period). Some types of diabetes medication may also need to be stopped before surgery.
This booklet includes advice on what to do with your medication just before and after the operation. With proper planning, these changes should not upset your diabetes control. If you have any difficulties understanding these instructions, please speak to a member of your local diabetes team, your pre-operative assessment nurse or your GP.
Blood glucose control
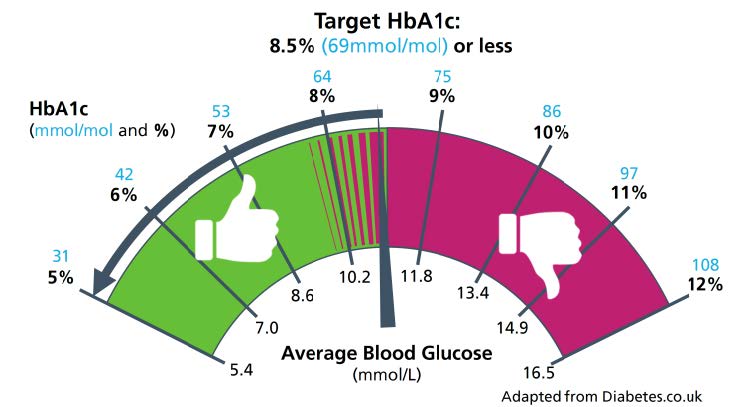
High blood glucose can increase the risk of infections and lead to less favourable outcomes following surgery. Good blood glucose control has also been shown to improve healing after surgery. HbA1c is a blood test that gives an overall picture of your blood glucose levels over the past 3 months. We recommend that your HbA1c should be 69 mmol/mol or less before your operation. For certain operations, a lower target HbA1c may be required. Your HbA1c will be checked at your pre-operative assessment and nurses will be able to advise you on the result. If it is high your surgery/procedure may have to be postponed until it improves. Your blood glucose will be checked on the day of the operation. If it is unstable, the healthcare team will aim to correct it first.
Fasting before surgery
For information about preparation before surgery, please see the leaflet given to you by your Pre-assessment Nurse.
- Surgery in the Morning
- If you are having surgery in the morning, you will be asked to attend the hospital at 07.15.
- Food and any other drink (tea, coffee, milk, juice etc.) can be taken until 02.30am
- You may drink water only from 02.30am
- At 06.00am please have a glass of water; please ensure you finish your glass of water by 06.30am.
- You should not suck any sweets or chew gum.
- Please bring all your regular medicines with you in the original containers. This includes all over-the-counter medicines, herbal preparations, ointments, creams and inhalers. You will be provided with a pharmacy bag to bring your medicines in.
- If you take any medication, the Pre- Assessment Nurse will advise you of the medication that should be taken at home on the morning of the day of your admission and surgery/procedure.
- Surgery in the afternoon
- If you are having surgery in the afternoon, you will be requested to attend the hospital at 11.45.
- You can have a light, early breakfast before 7.30am at home on the day of your admission and procedure. For example: two slices of toast, a bowl of cereal along with a cup of tea or coffee.
- Please make sure that once you have had your breakfast you do not eat anything.
- You may drink water only from 07.30.
- At 11.00am please have a glass of water; please ensure you finish your glass of water by 11.30am.
- You should not suck sweets or chew any gum.
- Please bring all your regular medicines with you in the original containers. This includes all over-the-counter medicines, herbal preparations, ointments, creams and inhalers. You will be provided with a pharmacy bag to bring your medicines in.
- If you take any medication, the Pre- Assessment Nurse will advise you of the medication that should be taken at home on the morning of the day of your admission and surgery/procedure.
Hypoglycaemia
If you have a reading below 4mmol/l this is called a ‘hypo’ and you may experience the following symptoms:
- Sweating, shakiness, dizziness, blurred vision, headache, fatigue, confusion, weakness
- Some people do not get symptoms, or get them at readings much higher than 4mmol/l. This is called ‘Impaired hypo awareness’. Please let staff know if you do not feel your hypos. If your glucose level is below 4mmol/l (This must be confirmed on a glucose meter) you need to take fast acting glucose (15-20g carbohydrate, even if you feel well). If you are fasting, it is recommended that you use a clear glucose juice (Lift juice) or 150 – 200 ml of clear apple fruit juice. Check your blood glucose again in 10-15 minutes and if still below 4mmol/L repeat your treatment if needed. Check again until your blood glucose is above 4mmol/L. Please let the staff know that you have done this when you arrive at the hospital.
Please remember to bring with you to hospital:
- This leaflet
- Hypo treatments
- Blood glucose testing equipment
- Diabetes medication (e.g., tablets, insulin) that you usually take for your diabetes.
- A supply of insulin needles (if you take insulin or other injectable treatment)
Insulin treated diabetes
On the day of your surgery, from 6 am onwards, you should monitor your blood glucose every 2 hours prior to your arrival at hospital and bring your record with you. If you are driving, you should also check your blood glucose just prior to starting your car and drive only if your blood glucose is more than 5 mmol/L.
Insulin Pumps: Please inform staff if you are on an insulin pump as some procedures can interfere with the function of the pump. Contact the diabetes team for MKUH on 01908 995 967 or [email protected] for a care plan to follow during your admission.
Changes to your diabetes medication
If you take medication for your diabetes (tablets or injectables), you may need to change the doses before your procedure. If you are not prescribed medication for your diabetes, you do not need to make any changes unless specifically advised to do so. By using the charts below your nurse may have specific instructions for you:
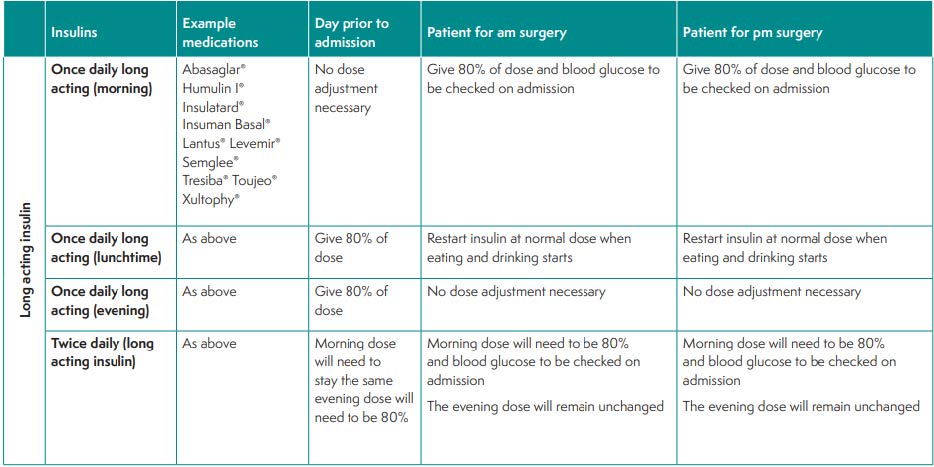
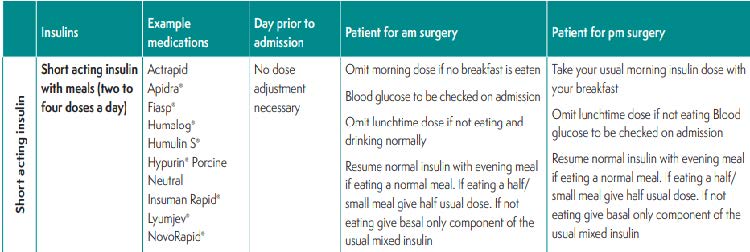
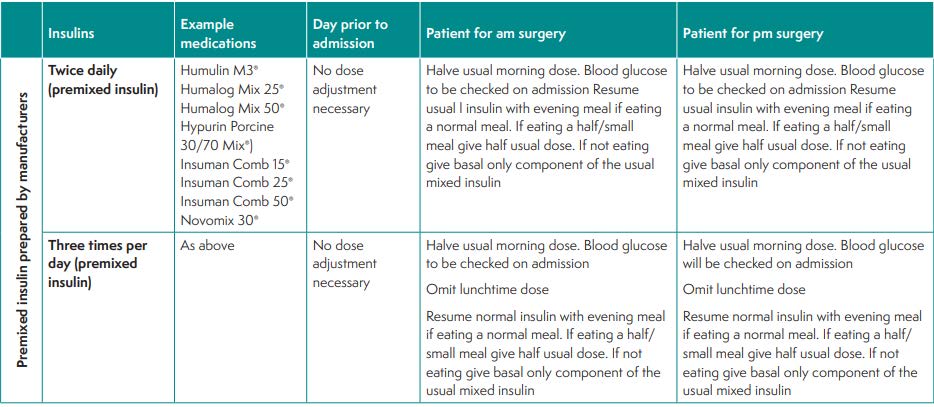
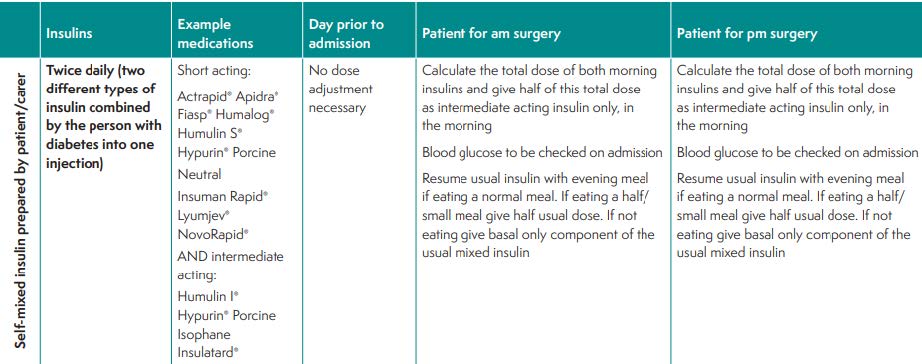
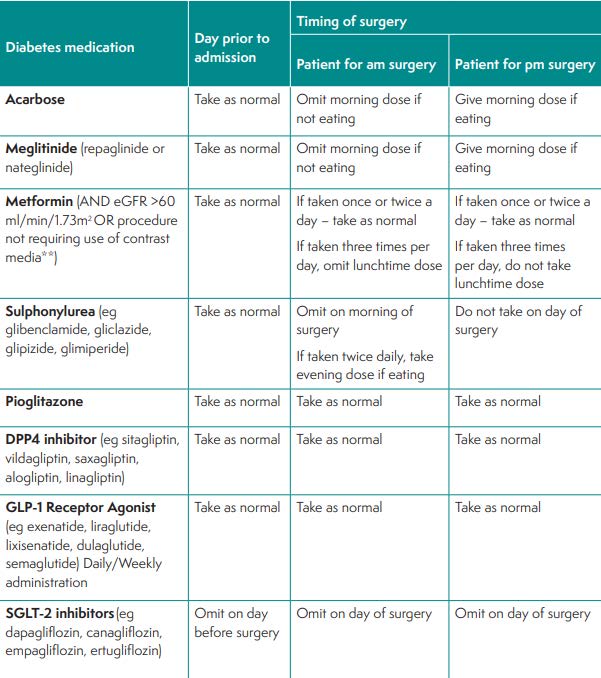
Tables taken from Perioperative Care of People with Diabetes Undergoing Surgery (CPOC 2022)
Insulin may need to be given via a vein in some circumstances. Your blood glucose will be checked hourly during this time. This will stop and normal medications resumed as soon as you feel well enough to eat and drink again. During your inpatient stay please refer to the leaflet ‘what to expect whilst in hospital’ and ask to be referred to the Diabetes Inpatient Nursing Team if you have any concerns. Please see our webpage for further information about diabetes management.
After your procedure
After your procedure, you will be offered food and drink when you feel able to eat. Once you are eating and drinking normally, you should resume taking your normal diabetes medication from that meal onwards. The healthcare team will be able to give you further advice on this.
At home:
- You should continue taking your usual diabetes medication (tablets or insulin) as advised by your healthcare team.
- Monitor your blood glucose levels if you usually do so or have the equipment – up to 4 times per day if possible (before meals and before bed).
- Your blood glucose levels may be higher than usual for a day or so—this is not a worry unless you are feeling unwell.
- If you become unwell, especially if you are vomiting and unable to eat or take medication. Contact your usual diabetes team/GP surgery or 111. Please ensure you let them know you just had surgery.
Follow up on your diabetes care
You should be informed if you require further diabetes follow-up, either by your surgery or by a member of your Diabetes team. If no follow-up is required, you will need to monitor your diabetes and continue to attend your GP surgery for your usual appointments.
