Hysteroscopy Under General Anaesthesia
Please note, this page is printable by selecting the normal print options on your computer.
This information sheet has been provided to you to help answer some of the questions you may have about having a hysteroscopy under general anaesthesia. It explains the benefits, risks and alternatives to the operation. If you have any questions or concerns, please feel free to speak with your doctor/nurse.
What is hysteroscopy?
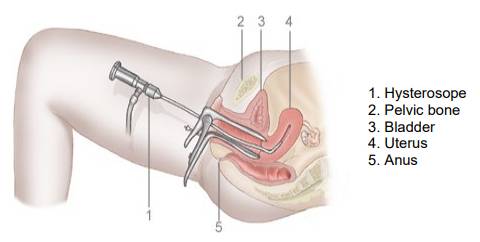
Hysteroscopy is a simple investigation that involves looking into the uterus (womb) with a telescope called a hysteroscope. Because the hysteroscope is inserted through the vagina, no incision to the abdomen, cervix or uterus is required.
Why do I need a hysteroscopy?
A hysteroscopy can help to find the cause of the problems you are having, such as:
• heavy vaginal bleeding
• irregular periods
• bleeding between periods
• bleeding after sexual intercourse
• bleeding after menopause
• persistent discharge.
• It is also used when abnormalities of the uterus are found during an ultrasound scan such as polyps (fleshy tissue protruding from the endometrium) fibroids (swellings that arise from the muscle of the uterus).
Hysteroscopy may also be advised when the uterus appears to have an abnormal shape. Minor procedures may be done at the same time to treat your condition, these may include:
• To remove, insert or change an intra-uterine contraceptive device (IUD).
• Removal of polyps or fibroids.
Are there any alternative treatments?
This procedure is also performed under local anaesthesia in the out-patient hysteroscopy clinic. An ultrasound can also be performed to look at the uterus (womb) and the lining of the womb, but it does not give us as detailed information as the hysteroscopy and therefore does not replace a hysteroscopy.
What about my periods?
If you are menstruating or are due to be menstruating at the time of your hysteroscopy don’t worry. Unless you have particular objection it is usually still possible to proceed.
Pregnancy test
To make sure that the procedure does not disturb a pregnancy, all sexually active women of child bearing age will be asked to provide a urine specimen to perform a pregnancy test on the day of the procedure. Your procedure will be cancelled if there is any possibility that you might be pregnant. Please use a barrier method of contraception, such as a condom or diaphragm, from your period before the procedure to the day of the procedure.
What happens during the procedure?
An instrument, called a speculum, is placed within your vagina to help the doctor see your cervix (the neck of the uterus). A speculum is the same instrument used during a cervical smear. Your cervix may then be opened slightly using a smooth instrument called a dilator. The hysteroscope is very narrow and is passed through the cervix into the cavity of the uterus. As the uterus is usually ‘folded up’, some fluid (normal saline) is introduced to ‘open up the womb’ so that the doctor can have a clear and direct view of the inside of the womb.
Any irregularities or growths can be seen, as well as the internal openings of the fallopian tubes. A small piece of tissue (biopsy) may be taken for examination by a pathologist. The procedure takes about 10 to 30 minutes. If you are being treated for fibroids or polyps, a special hysteroscope with an electrical loop, known as a resectascope will be used to remove them. If you have a general anaesthetic, you will be asleep during the entire procedure. When you wake up, you might feel some mild, abdominal (tummy) pain or cramps, which is similar to a period pain. Some discomfort is to be expected after the procedure and we will give you pain relief for this.
What are the benefits?
Hysteroscopy allows diagnoses as well as treatment of bleeding symptoms under direct vision.
What are the risks?
There are risks associated with any procedure. Your surgical team will explain these risks to you before you sign the consent form. Please do not hesitate to ask questions if you are uncertain.
Problems that can happen are:
• Accidental damage to the womb or cervix, this occurs in around 1 in 135 cases.
• The risk is slightly greater in postmenopausal women and in women who have recently been pregnant. This seldom causes any damage to other organs within the tummy cavity (abdomen) but does prevent the cavity of the uterus from being viewed.
• In the unlikely event that perforation does occur, the procedure would have to be abandoned .Sometimes a laparoscopy may be required, which is a procedure during which a camera is passed through your belly button to have a closer look inside your tummy cavity.
• Bleeding
• Pelvic infection is a rare complication of this investigation. Antibiotic treatment is usually effective in treating any infection.
• Failure to visualise uterine cavity.
• Although the procedure is performed with equipment that has been sterilised there is always the risk of an infection. If during the next five days you experience any of the following, please see your GP:
– A smelly vaginal discharge
– Heavy prolonged bleeding
– A temperature
– Feeling generally unwell/off colour
What happens after the procedure?
You might feel some mild, period like cramps or period like bleeding. Some discomfort is to be expected after the procedure and you can take pain relief (such as paracetamol) as instructed. We advise you to use sanitary towels and not tampons during this episode of bleeding to reduce the risk of infection.
Recovering from hysteroscopy
After your hysteroscopy, while you are still under the effects of the anaesthetic, you will be taken to the Recovery Room where you will be monitored by the recovery staff until you are transferred back to the ward. Back on the ward the nursing staff will monitor you and take routine observations. Your doctor will consult with you to explain how the surgery went and what the findings were.
Leaving hospital
You will usually be discharged from hospital the same day as the procedure. Your doctor will give you the relevant instructions for looking after yourself during the post-operative period.
When can I have a bath or shower?
You can have a shower on the day of the procedure and a bath the next day. If you have had a general anaesthetic, you might feel dizzy so please have an adult around to help you, if needed, and keep the bathroom door unlocked.
When can I have sexual intercourse?
Please do not have sexual intercourse until after your next period, to help prevent an infection in the uterus or vagina.
How long will it take me to recover?
Every patient reacts differently to anaesthetic and there is no definite rule as to when you can return to work or start physical activities e.g. running, swimming etc. It is advisable to have some rest to help you heal and to let the anaesthetic wear off properly. Please do not return to work or perform strenuous exercise until you feel ready to do so. Please let the nursing staff know if you need a sick note.
When can I get the results?
If a biopsy has been taken, we send it to a special laboratory in the hospital for tests. We will usually let you have the results by post or at the follow-up appointment.
Questions or concerns:
If you have any questions or concerns, please contact:
Urgent Care Centre 01908 303030
Day Surgery Unit (DSU) 01908 995468 / 995469 (0700-2000)
Further information:
The following website contains further information about this procedure: http://www.nhs.uk/Conditions/Pages/bodymap.aspx
