Hysterectomy
Please note, this page is printable by selecting the normal print options on your computer.
What is a hysterectomy?
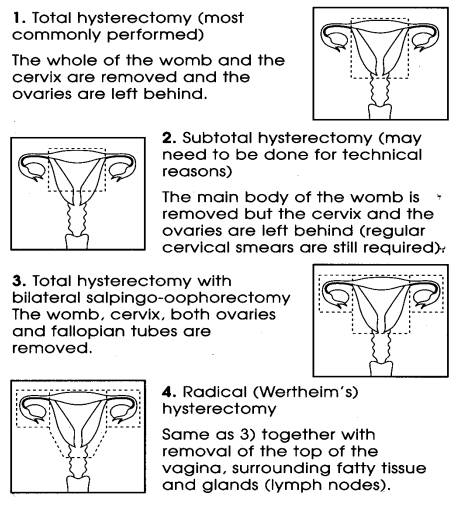
A hysterectomy is an operation to remove the womb. The operation may also involve removal of one or both of the Fallopian tubes and ovaries, and also may include removal of the cervix.
What types of hysterectomy are there?
There are three main types:
Abdominal hysterectomy – This is the most common and is performed by cutting open the lower abdominal wall usually along the bikini line. If there is a large cyst or fibroids the incision may be vertical.
The abdominal approach – the skin on your abdomen [tummy] will be cleaned with antiseptic, the incision will be made and the uterus removed by clamping and cutting large blood vessels and tying them off. The top of the vagina is then either closed or left open to drain fluid and blood. Each layer of tissue of your abdomen is individually stitched until the wound is completely closed and finally subcutaneous dexon (dissolvable suture), metal clips or nylon sutures are used. The metal clips or nylon sutures are usually removed 5-7 days post operatively.
Vaginal hysterectomy – this means the operation is performed through the vagina. The advantage of this type of hysterectomy is that no cut is made in the abdomen so there are no visible scars; however, it is not suitable for all women. Vaginal hysterectomy involves a shorter hospital stay and more rapid recovery. In the UK about one quarter of all hysterectomies are performed vaginally, but in some cases where the uterus is very large because of fibroids, a vaginal hysterectomy is impossible.
Laparoscopic Hysterectomy [Keyhole Surgery]
A laparoscope [telescope] is inserted into the abdomen to view pelvic organs; this avoids the need for large abdominal incisions. Two or three further incisions are made to insert instruments to carry out the procedure. The uterus is removed vaginally. The advantage of the laparoscopic hysterectomy is that it is a less invasive operation than an abdominal hysterectomy and the recovery is much quicker.
Why a hysterectomy?
Hysterectomies are performed for a variety of reasons, including:
• Heavy bleeding – due to hormone imbalance where less invasive treatment ( Mirena coil, endometrial ablation) options have failed, fibroids.
• Fibroids – these are benign [non cancerous] muscular growths in the womb [uterus]. 20% of women over the age of 30 have at least one fibroid.
• Pain – severe period pains, pelvic inflammatory disease which causes pain. Endometriosis also causes chronic pain and scarring. A hysterectomy is no guarantee that pelvic pain will be cured.
• Prolapse – dropped womb. This happens when the front and back walls of the vagina, the pelvic floor muscles and supporting ligaments of the womb become weakened.
• Cancer – Cancer of the cervix, endometrium [cancer of the womb], cancer of ovary. The chances of a cure are very good if a cancer is diagnosed early enough.
A hysterectomy may be necessary to treat your individual problem. However, there may be other options such as medication, either by mouth or directly into the uterus (Mirena – Intra-uterine system). Laser or Thermal ablation treatment which destroys the lining of the womb works for some people but it is not a guaranteed cure, up to 20% of women need further treatment. A hysterectomy is a major operation. It takes 3 months to fully recover, however, after that there are no more periods.
What are the risks of hysterectomy?
For most women, having a hysterectomy will not cause any problems. However, some women may suffer with a slight fever or difficulty in emptying the bladder for a couple of days after the operation. More serious complications such as infection, bleeding and damage to the bowel, bladder or ureters are very rare. In addition there are the anaesthetic risks, adhesions from surgery causing pain and the risk of developing a DVT/PE [Deep Vein Thrombosis/Pulmonary Embolism].
What steps are taken to minimise these risks?
Your surgeon may advise that you have an injection of antibiotics into your drip during surgery. Bleeding can usually be controlled by careful stitching; occasionally a blood transfusion can be necessary. If you would not accept that, you should discuss it with your gynaecologist in advance. You can help yourself to avoid the risk of complications by stopping smoking, eating a healthy varied diet, taking regular exercise and being of normal weight for your height as you prepare yourself for surgery.
What happens before the operation?
Pre-Operative Assessment – The clinic provides the opportunity to assess you fully and gather all the information required to make an informed decision regarding your fitness for surgery. You will be informed about what will be happening to you during your surgery, e.g. the surgical/and anaesthetic techniques, what will happen in the anaesthetic room and recovery area, what drips, drains and tubes you will wake up with and how post-operative and post discharge pain will be controlled.
Hospital Admission
You will normally be admitted to the hospital ward the day of the operation. In some circumstances laxatives are advised to ensure the bowel is empty before surgery. You will have your legs measured for support stockings to wear during and after your operation [this reduces the chance of blood clots forming in the veins of your legs]. An anaesthetist will visit you to ask some questions about your general health and ensure you are fit for surgery. If you have any concerns remember to ask the anaesthetist at this time. You will then be asked to put on a theatre gown and the support stockings as mentioned earlier.
The Operation
Once in the anaesthetic room a fine plastic tube will be positioned into your hand to give you the anaesthetic drugs. Blood pressure cuff and ECG electrodes will be fitted as routine procedure to monitor you during your surgery. In some cases a general anaesthetic is not given and a spinal anaesthetic is used instead. The anaesthetist will discuss this with you prior to surgery.
After the Operation
When you wake up you will find that a drip has been placed in your arm to give you fluids, and a small tube [catheter] may also have been inserted into your bladder to help it drain. You may also have a drainage tube coming from near the wound this drains any excess fluids that may come from your operation site. This is done to help aid your recovery for 24-48 hours. As you recover you will have your blood pressure and pulse rate taken regularly. If you are in pain then ask the nurse for painkillers as necessary.
You are likely to feel uncomfortable but this will begin to lessen over the next few days. You will be encouraged to sit up and get out of bed the day after your operation or as soon as you are able. The physiotherapist may visit you to explain simple breathing exercises to help with coughing and other exercises to help get your muscles back into shape if required. A small amount of discharge or bleeding from the vagina is perfectly normal, if any heavy bleeding occurs, tell the nurse.
After a day or so you should feel like eating and drinking again and the drip in your arm and the catheter into your bladder will be quickly and easily removed. Depending on which type of hysterectomy you have had, you will be in hospital for a total of between 2 and 5 days and rarely more than 7 days.
Aftercare at home
You should get plenty of rest for the first two weeks after your operation but make sure you try to have a walk each day, never overdoing it and gradually increasing the distance. If you are given painkillers to take home, it is important for your recovery that you take them regularly as prescribed. Avoid strenuous exercise for 3 months. Have a bath or shower daily, if you have an abdominal wound ensure it is dried thoroughly and inspected for signs of infection such as: redness, discharge or an increase in pain around the area.
You may have bleeding/spotting from the vagina for up to two weeks following surgery. Be aware of any offensive discharge or heavy bleeding as this may indicate an infection and your GP should be consulted. After three or four weeks you can drive again although it is a good idea to have someone in the car with you. You must be confident that you will be able to do an emergency stop before you start driving, and that your insurance company will cover you after this time.
Be very careful with housework – do not lift anything heavy for 3 months. Try to do things sitting down and avoid standing for long periods. Every woman is different in how long it takes her to get better after this operation. In general you should be fine to go back to work any time after 6-12 weeks. Your doctor will advise you when you are fit enough to do so. If at any time either before or after the operation there is something which you do not understand or questions you want to ask then do not hesitate to talk to the doctor or the nurse.
Sex after a hysterectomy
Sexual intercourse may resume when you feel that you are ready. You may bleed from the stitch lines at the top of the vagina if resumed too quickly. Take your time and do what feels comfortable for you. If you had previously experienced pain because of the condition you had, then your sex life after the operation may be enhanced. If vaginal dryness is a problem try a lubricant such as KY Jelly. It is not clear what impact hysterectomy has on sexual function. For many women who had long/heavy periods or pelvic pain it is greatly improved. Sometimes women need reassurance of their femininity and sexuality after having a hysterectomy.
HRT [Hormone Replacement Therapy]
If you have had your ovaries removed, you will have an artificial menopause, which may result in hot flushes, night sweats, vaginal dryness and skin irritation. These symptoms can be controlled with HRT. Make an appointment to discuss HRT with your GP.
Further information:
People are unique and the alternative, risks and benefits will of course vary from person to person. We hope this leaflet will support the information you have already received from your doctor in enabling you to make an informed decision about your care.
