Good Bowel Habit and Preventing Constipation
Please note, this page is printable by selecting the normal print options on your computer.
This leaflet has been designed to promote good bowel habit and to prevent constipation.
Good Bowel Habit
Many anal and rectal (bottom and back passage) problems are caused by poor bowel habit. The most effective time to empty your bowel is when you first get the urge to go. First thing in the morning or following a meal are common times to get this urge. Do not strain to empty the bowel. Straining pushes down on the muscles supporting your pelvic area, preventing the bowel from
emptying effectively. Straining also pushes out haemorrhoids (piles). Opening the bowels should take no more than two or three minutes and the faeces (sometimes known as stools or motions) consistency should be semisolid, like toothpaste.
How often should I empty my bowels?
There is no right or wrong answer to this. There is a very wide range of “normal” bowel function between different people. It is not essential to have one bowel action per day, and indeed it is probably a minority of the total population who has this. Some people always empty their bowels several times per day; others have several days between bowel actions. Understanding of what is normal is based on personal experiences and growing up with other people. Most of us do not discuss our bowel habit with our friends, or even our family. A few people become obsessed with the need for a daily bowel action and spend large amounts of time in the toilet or take laxatives to achieve this. This is unnecessary.
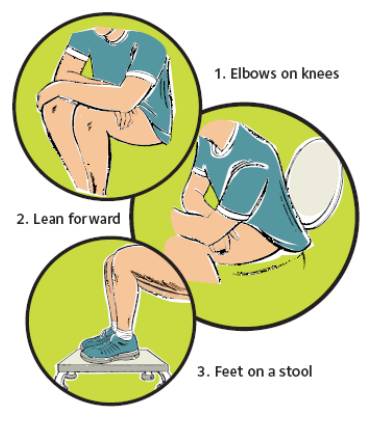
How to open your bowels – the perfect position
How to open your bowels – the right actions
1. Abdominal bracing (making your waist wide).
2. Relax and bulge the tummy muscles.
3. Let go – without straining, relax and widen the back passage. Do NOT hold your breath.
4. Finish – draw up the back passage firmly.
Ideas to ensure that you have the best chance of passing Faeces (stool)
• Try to go to the toilet at a regular time or times every day. This may follow breakfast or a coffee.
• Take your time. Try to ensure that you will have about 10 minutes without interruption.
• Firstly make sure you are comfortable on the toilet. It is most natural for humans to squat to pass a stool. You may find that having your feet on a footstool about 20-30 cm (8-10 inches) high helps by improving the angle of the rectum within the pelvis, making it easier to pass stools (see diagram above). Keep your feet about 1.5 – 2 feet apart.
• Relax and breathe normally. Do not hold your breath as this will encourage you to strain.
• Using your abdominal muscles effectively is best done with one hand on your lower abdomen, and one on your waist. As your abdominal muscles tighten you should feel your hands being pushed out forwards and sideways. This is called ‘brace’ or ‘brace and bulge’.
• Concentrate on relaxing the anus to allow the stool to pass. Do not push from above without relaxing the anus below.
• Do not adopt any “weird and wonderful” positions – this will not help you in the long-term.
• Do not spend endless time on the toilet straining. If the bowels do not open – do not panic – try again at the same time the next day. It may not be normal for you to pass faeces (a stool) every day.
Constipation in Adults
A common cause of constipation is not eating enough fibre. Less common causes include a side-effect from medicines, and certain medical conditions. In many cases the cause is not clear. The most common treatment and prevention of constipation is to eat plenty of fibre, and to drink plenty. Laxatives are sometimes needed but, ideally, should only be used for short periods of time until symptoms ease.
What is constipation?
Constipation is common. If you are constipated it causes one or more of the following;
• Faeces (sometimes called stools or motions) become hard, and difficult or painful to pass.
• The time between toilet trips increases compared to your usual routine. (Note: there is a large range of normal ‘bowel habit’. Some people normally go to the toilet to pass faeces 2-3 times per day. For others, 2-3 times per week is normal. It is a change from your usual pattern that may mean that you are constipated.)
• Sometimes crampy pains occur in the lower abdomen. You may also feel ‘bloated’ and feel sick if you have severe constipation.
What are the causes of constipation?
• Not eating enough fibre (roughage) is a common cause. Fibre is the part of plant food that is not digested. It remains in your gut. It adds bulk to the faeces, and helps your bowels to work well. Foods high in fibre include: fruit, vegetables, and cereals.
• Not drinking much may make constipation worse. Your faeces will usually be soft and easily passed if you eat enough fibre, and drink enough fluid. But note: there is great variation. Some people need a lot more fibre and/or fluid than others in order to avoid constipation.
• Some special ‘slimming diets’ are low in fibre, and may cause constipation.
• Some medicines can cause constipation as a sideeffect. For example: painkillers (particularly those with codeine such as co-codamol), some antacids, some antidepressants, iron tablets, morphine, but there are many others. Tell a doctor if you suspect a medicine is making you constipated. A change of medication may be possible.
• Various medical conditions can cause constipation. For example, an underactive thyroid, irritable bowel syndrome, and conditions that cause poor mobility, particularly in the elderly.
• Pregnancy. About 1 in 5 pregnant women become constipated. It is due to the hormone changes of pregnancy that slow down the gut movements.
• Emotion. Some people say that ’emotional problems’ can lead to constipation, but this is hard to prove or to measure.
• Unknown cause (‘idiopathic’). Some people have a good diet, drink a lot of fluid, do not have a disease which can cause constipation, but become constipated. Their bowels are said to be ‘underactive’. This is quite common. Most cases occur in women. This condition tends to start in childhood or in early adulthood, and persist throughout life.
Do I need any tests?
Usually not. However, tests may be advised if you have any of the following:
• If regular constipation is a new symptom, and there is no apparent cause such as a change in diet, lifestyle, or medication.
• If symptoms are severe and persistent.
• If other symptoms develop. For example, if you pass blood from your bowel, or have pain, weight loss, bouts of diarrhoea, or other unexplained symptoms in addition to constipation.
What can I do to help myself and to prevent constipation?
• Eat plenty of fibre by eating plenty of fruit, vegetables, cereals, fruit juice, wholemeal bread, etc. See below. (Note: a high fibre diet can make the situation worse in some people with severe
longstanding constipation. But this is rare. See below in the section ‘bulk forming laxatives’ for an explanation).
• Have plenty to drink – at least two litres (about 8-10 cups) of fluid per day. You will pass much of the fluid as urine, but some is passed out in the gut and softens the faeces. Most sorts of drink will do, but alcoholic drinks can be dehydrating and may not be so good.
• Exercise regularly if possible. Keeping your body active helps to keep your gut active.
• Toileting – Do not ignore the feeling of needing the toilet. Some people suppress this feeling if they are busy. It may result in a backlog of faeces forming that are difficult to pass later.
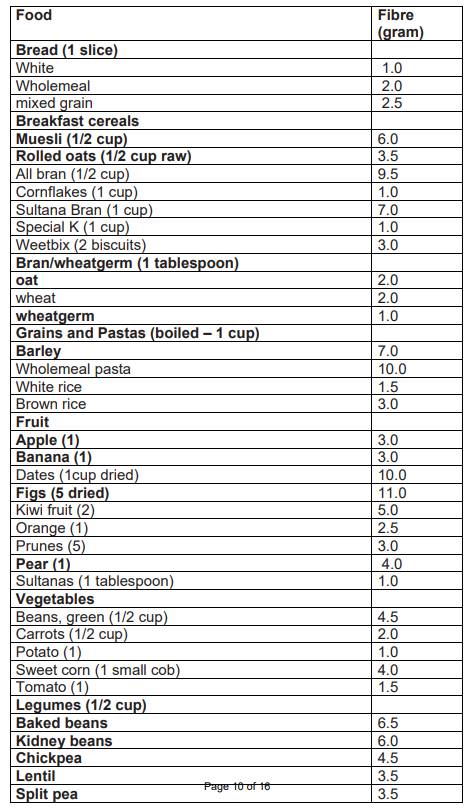
Examples of fibre rich foods
You should aim to eat 25-35 grams of fibre a day and it should be a mixture of soluble and insoluble fibre. Those sources of fibre in bold are soluble fibre, those not in bold are insoluble fibre.
What are the treatments for constipation?
Treatment with a laxative is needed only if the measures above (fibre, fluid, etc) do not work well. There are four main groups of laxatives that work in different ways:
• Bulk-forming laxatives (sometimes called fibre supplements).
• Stimulant laxatives.
• Osmotic laxatives.
• Faecal (stool) softener laxatives.
There are various types and brands in each group. The one recommended to you depends on factors such as your own preference, possible unwanted effects, other conditions that you may have, and cost. You can buy some laxatives at pharmacies, and get them all on prescription if needed. The different groups are briefly discussed below. Note: as a rule, you should use a laxative only for a short time, when necessary, to get over a bout of constipation. Once the constipation eases, you should normally stop the laxative. Some people get into the habit of taking a laxative each day to ‘to keep the bowels regular’ or to ‘prevent constipation’. This is not advised, especially for laxatives which are not ‘bulk-forming’. If you feel that you need a laxative regularly, then see a doctor for advice on which is best to use in your circumstances. (Some people with persistent and severe constipation do require regular laxatives. But it is best if this is done under the advice and supervision of a doctor).
Bulk-forming laxatives (sometimes called fibre supplements)
These increase the ‘bulk’ of your faeces similar to fibre. They can have some effect within 12-24 hours. However, their full effect may take some days to develop. Alternatives are ispaghula husk, methylcellulose and sterculia.
A note of caution: fibre and bulk-forming laxatives partly work by absorbing water (a bit like blotting paper). The combination of bulk-forming laxatives and fluid usually produces soft, bulky faeces which should be easy to pass out.
When you eat a high fibre diet or take bulk-forming laxatives:
• You should have plenty to drink. At least two litres per day (8-10 cups). Your faeces may become dry and difficult to pass if you do not have enough to drink. Very rarely, lots of fibre or bulk-forming laxatives and not enough fluid can cause an obstruction in the gut.
• You may notice an increase in wind (flatulence) and abdominal bloating. This is normal and tends to settle down after a few months as the gut becomes used to the increase in fibre (or bulk-forming laxative). Occasionally, bulk-forming laxatives can make symptoms worse if you have very severe constipation. This is because they may cause abdominal bloating and discomfort without doing much to clear a lot of faeces which are stuck further down the gut. See a doctor if you feel that bulk-forming laxatives are making symptoms worse.
Stimulant laxatives
These stimulate the nerves in the large bowel (the colon and rectum). This then causes the muscle in the wall of the large bowel to squeeze harder than usual. This pushes the faeces along and out. Stimulant laxatives include senna, bisacodyl, and dantron. These usually take effect within 8-12 hours. Therefore, a bedtime dose is recommended so you are likely to feel the urge to go to the toilet the following morning. Stimulant laxative suppositories act more quickly (within 20-60 minutes). Possible side-effects from stimulant laxatives include abdominal cramps, and a ‘lazy bowel’ with long-term use.
Osmotic laxatives
These work by retaining fluid in the large bowel by osmosis (so less fluid is absorbed into the bloodstream from the large bowel). A commonly used one is called lactulose. However, this can take up to two days to have any effect so it is not suitable for the rapid relief of constipation. Possible side-effects of lactulose include abdominal pain and bloating. Some people find the taste of lactulose unpleasant. Another osmotic laxative is called polyethylene glycol (trade name Movicol). This usually has a rapid action.
Faecal softeners
These work by ‘wetting’ and softening the faeces. The most commonly used is docusate sodium (which also has a weak stimulant action too). Bulk-forming laxatives also have some faecal-softening properties. Liquid paraffin used to be commonly used as a faecal softener. However, it is now not recommended as it may cause side-effects such as seeping from the anus and irritating the skin, and it can interfere with the absorption of some vitamins from the gut.
Other treatments
Constipation is usually helped by the above treatments. Sometimes, an enema is needed in severe cases. Other treatments may be advised by a specialist for people with severe constipation who have not been helped by the treatments listed above.
Some text copyright EMIS and PiP 2007 as distributed on www.patient.co.uk, table copyright Commonwealth of Australia, used with permission.
