Glycaemic Index (GI)
Please note, this page is printable by selecting the normal print options on your computer.
What is the Glycaemic Index (GI)?
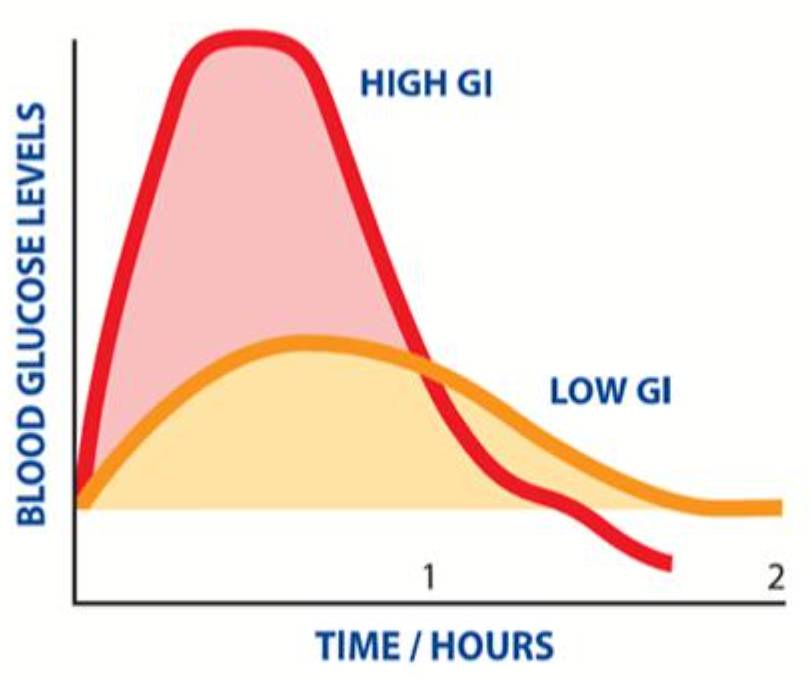
The glycaemic index (or GI) ranks foods based on how quickly they cause a rise in blood sugar (glucose) levels after eating.
Each time you eat or drink something containing carbohydrate, your blood glucose levels rise. Some foods containing carbohydrate are digested and absorbed quickly and cause a rapid rise in blood glucose levels; these are known as high GI foods. Lower GI foods are digested more slowly, which makes your blood sugars rise more slowly and gradually. The GI of a food is usually described as high, medium, or low.
The GI of a food is not dependent on the amount of total carbohydrate present in the food but on the structure of the carbohydrate and how complex this is. More complex structures of carbohydrate, such as cereals with grains or seeds have a lower GI.
How to use GI?
The GI value of a food is calculated when a food is eaten on its own. We generally eat items of food in combination with other foods, so it is important to look at the GI of the whole meal or snack rather than the individual GI values of each food. It is essential to assess GI within the context of a varied balanced diet. The total amount of carbohydrate eaten has the largest effect on blood sugar levels.
High GI foods do not need to be avoided but you should consider eating smaller portions of these foods, as well as the other foods they are eaten with. Mixing high GI foods with lower GI foods (e.g. fruit, vegetables and protein rich foods), will lower the overall GI of the meal.
Foods which are high GI are not necessarily unhealthy foods and low GI foods are not always healthy options. For example, chocolate and ice cream have a low GI.
What factors affect the GI of a meal?
- Cooking and processing methods – which will start the breakdown of the carbohydrate structure in foods.
- Ripeness of fruit and certain vegetables. The riper they are, the higher the GI of that food becomes.
- Wholegrains and high fibre foods act as a physical barrier to slow down absorption of carbohydrate by the body. This is not the same as ‘wholemeal’, where even though the whole of the grain is included, it has been ground up instead of left whole. So, some mixed grain breads that include wholegrains such as seeded bread have a lower GI than either white or wholemeal bread.
- Fat lowers the GI of a food. For example, chocolate has a low GI because of its fat content and crisps have a lower GI than potatoes cooked without fat.
- Protein lowers the GI of food.
- The combination of foods with different GI Values – adding one low GI food – will lower the GI of the whole meal.
- The meal size – A larger amount of carbohydrates will take longer to digest, and will have a greater impact on your blood sugars also referred to as glycaemic load.
Why should I think about GI?
To achieve the best possible blood glucose levels after meals, the correct amount of insulin for the carbohydrate you eat is essential.
Injected insulin works too slowly to deal with the glucose rise from high GI foods. The profile of insulin matches best with lower GI foods. Evidence shows that diets that contain more low GI foods help achieve better overall blood glucose levels and long-term health.
Aim for at least 1 low GI food item in each meal. High GI foods do not need to be avoided but consider eating smaller portions as well as what foods they are eaten with. For individuals with Type 1 Diabetes, high GI foods are required for treatment of hypoglycaemia and can be useful with exercise management.
How do I lower GI?
Remember – Adding a low GI food to a meal will lower the glycaemic index of the whole meal. The more often you can use low GI options within a meal or snack, the greater the benefits.
Some suggestions for you to consider:
Breakfast –
Try adding fruit to cereal.
Use a combination of cereals, one of which contains oats.
Include yoghurt.
Lunches –
Add baked beans to jacket potatoes.
Soups – try those with lentils or beans included.
Have a variety of breads – use pitta, wraps or seeded multigrain types.
Include salad or vegetables (e.g. raw carrot, celery sticks in a lunch box, etc.).
Main meals –
Use pasta, basmati rice or noodles with meals.
Try sweet potato in combination with ordinary potatoes.
Add pearl barley, beans, or lentils to casseroles.
Always have plenty of vegetables.
Have fruit and yoghurt as part or all your dessert.
Snacks –
Fruit, vegetables sticks, yoghurt, popcorn, glass of milk
For more information see: https://glycemicindex.com/
Information leaflet produced with kind support of Oxford Children’s Diabetes Team.
