Gastroscopy with Oesophageal Stent Inserted
Please note, this page is printable by selecting the normal print options on your computer.
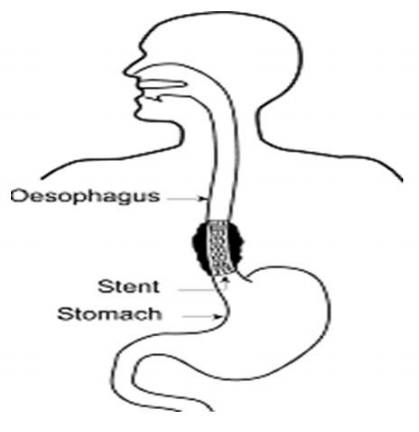
The oesophagus or gullet is a hollow muscular tube which takes food from the mouth to the stomach. If it becomes narrowed or blocked, then there will be a problem with swallowing. One way of overcoming this problem is by inserting a metal tube called an oesophageal stent.
This procedure requires your formal consent. This booklet has been written to enable you to make an informed decision in relation to agreeing to the investigation. You will be required to sign a consent form on the day of the procedure, which is a legal document, therefore please read this booklet carefully beforehand. If you are unable to keep your appointment, please notify the endoscopy unit as soon as possible.
This will enable staff to give your appointment to someone else and to re-arrange another date and time for you. You need to understand all the information, including the possibility of complications. There will be the opportunity to speak to a health care professional about anything that you do not understand on the day of the procedure before you sign the consent form.
What is a Gastroscopy with Oesophageal Stent inserted?
A Gastroscopy (which is also sometimes called an Upper Gastro-Intestinal endoscopy) involves putting a tube through the mouth into the oesophagus (gullet), down through the stomach and into the first part of the intestine (duodenum). By doing this the doctor can examine the upper digestive tract to detect any abnormality. A stent is a flexible, fine, metal mesh tube. It is inserted via the gastroscope into the oesophagus (gullet) and positioned across the area that has narrowed.
Are there any alternatives to having a stent inserted?
The aim of the stent is to allow you to swallow more easily again. If you decided against having this procedure and you can no longer swallow the nutrition the normal way; there are alternatives available, but these are not appropriate for everybody. You’ll need to discuss these with your consultant.
How do I prepare?
To get a clear view of the oesophagus and stomach it is important that the stomach is empty. Please do not eat or drink anything for at least six hours before the procedure.
What about my medication?
Routine Medication: If you are on any medication, especially blood pressure tablets, you should take these with a sip of water as usual.
Diabetes: If you have diabetes and control this with insulin or tablets, please ensure that the Endoscopy Unit is aware so that your procedure can be booked for the beginning of the list. You will need to stop your diabetes medication during your “Nil by Mouth” phase. Your usual medication can be recommenced after the procedure once you are eating again. You may want to bring a sandwich with you to eat after the procedure with your usual diabetes medication.
If you have any further concerns, please contact your diabetic specialist nurse well in advance of the procedure for advice.
Anticoagulants/ Antiplatelets: If you are taking blood- thinning medicines, such as Warfarin, Dabigatran, Heparin, Deltaparin, Apixaban, Clopidogrel, the dose of these may need to be altered or stopped before your procedure. You may also need to have blood tests before your procedure. If the referring doctor did not give you instructions, you may be referred to the bridging clinic for advice on stopping your medication. If this is required, this will be arranged for you by the referring clinician or the endoscopy booking coordinator.
What to bring with you?
Along with your appointment letter you will have received a health questionnaire. Please complete it and bring it with you. You will also find enclosed a copy of your consent form; please read this carefully but do not sign it. This is just an example for you to read carefully prior to your appointment. The endoscopist will meet with you prior to your endoscopy to discuss what is going to happen, any risks and any serious or common side effects. At this point you will be given the opportunity to ask any questions and then you will sign the ‘actual’ consent form.
Bring everything you may need for an overnight stay in hospital.
How long will I be in the Endoscopy unit?
Please note that the time of your appointment is not the time that the procedure will be performed. How long you will be in the unit will depend on how quickly you recover from the procedure, the sedation you may have had and on how busy the unit is. The unit also looks after emergencies, and these can sometimes take priority over outpatient procedures. You should be kept informed of any delays, but if you have any questions or concerns, please ask a member of the staff.
Once your observations are stable, you will be transferred to a ward for an overnight stay.
What will happen when I arrive?
You will be admitted to hospital on the morning of your procedure. This is so that you can be seen by a doctor and have blood tests taken before you have the procedure.
Before you have the procedure, the doctor will ask you to sign a Consent Form. He will explain the procedure again and answer any questions you may have. He will also explain any potential risks.
Sedation
Usually, an intravenous sedation is offered for this procedure, you can discuss this with the endoscopist before the procedure. A sedative (usually Midazolam) and/or a painkiller (Fentanyl or Pethidine) may be offered which will be administered through an IV cannula (a plastic tube) which is inserted in a vein in your arm/hand. This will make you slightly drowsy and relaxed, but not make you go to sleep like a general anaesthetic. You will still hear what is said to you and therefore, will be able to carry out simple instructions during the procedure. Some people do not remember anything about the procedure once the effects have worn off.
Whilst you are sedated, we will monitor your breathing, respiration, and pulse rate via a finger probe, so that any changes can be recorded and dealt with accordingly. You will also be given some oxygen via a nasal sponge into your nostril. Your blood pressure may also be checked and recorded.
You must arrange for a responsible adult to collect you once discharged.
You should not drive, return to work, operate machinery, or drink alcohol for 24 hours after the procedure, nor should you make any important decisions. The reason for this is that the sedation may, even though you may feel perfectly normal, still be in the body and may impair your judgement.
The Procedure
When it is your turn, you will be taken to the Endoscopy procedure room; you will be introduced to the team and a verbal safety checklist (called “WHO”) will be done. Your throat will be made numb by using the local anaesthetic spray; you will then be asked to lie on your left side. A “probe” will be placed on your finger which can read your pulse and the amount of oxygen in your body (pulse oximeter). Oxygen will be given, usually via a sponge which is placed into one of your nostrils. A mouth guard is placed lightly between your teeth. If you wear dentures these will be removed before the guard is inserted.
The Doctor passes a flexible tube (endoscope) down through your throat, into your gullet. A guide wire is inserted across the narrowing and then a stent is passed over the guide wire and position confirmed. Once the doctor is happy with the position, the stent will be released under x-ray control, and it will begin to gently expand. The endoscope is then gently passed to confirm the stent is in place. The procedure should take about 20 minutes.
Milton Keynes University Hospital is a teaching hospital and there may be a student and/or a trainee present in the room, or a supervised trainee may be doing your procedure. If you have any concerns or objections, please contact the Endoscopy Unit prior to your test or make the nurse admitting you aware of this.
Will it hurt?
Sometimes, during the procedure, people may experience chest or back discomfort/ pain, this usually settles within a couple of days. Please let your nurse and/or doctor know if you do have discomfort or pain as pain relief medication can be given to help you feel more comfortable.
Aftercare
After your procedure you may have a chest x-ray to check that your stent is in the correct place. The nurse will tell you when you are allowed to have a drink and something soft to eat. This may be a few hours after you returned to the ward.
Before you go home the Dietitian and/or your key worker (your Upper Gastro-Intestinal (UGI) Nurse Specialist) may come and talk to you about types of food you can have and give you some simple tips on how to keep your stent clean. This is mainly about having plenty of fluids to drink, particularly with your meals. Please be aware that there will be some types of food that you will still need to avoid.
Here are some simple tips:
- Sit upright to eat.
- take small mouthfuls of food.
- eat slowly and chew your food well.
- use plenty of sauces, gravy, and butter to moisten food.
- if your appetite is poor, consider having smaller and more frequent nourishing meals.
Are there any risks or complications?
Having an Oesophageal Stent inserted is a very safe procedure but like with any other medical intervention, it does have some risks and complication that can arise with it. We want to draw your attention to them in order to help you make your decision. The doctor or specialist nurse who has requested the test will have considered this already. The risks must be compared with the benefit of having the procedure carried out.
The possible complications of gastroscopy stent insertion are listed below. Any numbers which relate to risk are from studies of patients who have had this procedure. Your doctor will tell you if the risk of complications is higher or lower for you.
- Sore throat, which gets better quickly.
- Allergic reaction to equipment, materials, or sedative. The endoscopy team is trained to detect and treat any reaction that may happen. Let the admitting nurse and endoscopist know if you have any allergies or you have reacted to any drugs or tests in the past.
- Breathing difficulties or heart irregularities, as a result of reaction to sedation or inhaling secretions such as saliva. To help prevent this from happening, your respiration and oxygen levels will be monitored, and a suction device will be used to clear any secretions. Rarely, a heart attack or stroke (loss of brain function resulting from an interruption of the blood supply to the brain) can happen if you have serious medical problems.
- Aspirating fluid in airway (minor risk)
- Perforation – making a hole in the oesophagus, stomach, or duodenum (risk: between 2% and 5 %). The risk is higher if there are any abnormal narrowing (stricture) which is stretched (dilated). If a hole occurs, you will need to be admitted to hospital for further treatment which may include surgery.
- Damage to teeth and bridgework. The nurse will place a plastic mouthpiece in your mouth to help protect your teeth. Let the endoscopist and nurse know if you have any loose teeth or dentures.
- Bleeding from minor damage caused by the endoscope. The stent can sometimes cause minor bleeding during the procedure. Bleeding is rare and usually stops on its own.
- Incomplete procedure. This can happen due to a technical difficulty, food or blockage in the upper digestive system, complications during the procedure, or discomfort.
- Sedation. This can occasionally cause problems with breathing, heart rate and blood pressure. If these problems do occur, they are usually short lived. Careful monitoring by the endoscopy team ensures that any potential problems can be identified and treated quickly. Older patients and those with significant health problems, such as breathing difficulties due to a bad chest, may be assessed by a doctor or specialist nurse before having the procedure.
- It is not uncommon to feel some mild to moderate chest pain while the stent “beds in” but normally settles in a day or two.
- Some patients get heartburn after the procedure and need to take medication for this.
- Very rarely the stent may migrate out of position, and it is necessary to repeat the procedure.
- Complications can happen. Some of these can be serious and can even cause death (risk: 1 in 25,000).
You should discuss these possible complications with your doctor if there is anything you do not understand.
What if the stent becomes blocked?
When a stent becomes blocked it normally causes some discomfort or pain, difficulty with swallowing and sometimes regurgitation of food. Try not to panic. The following actions may help:
- stop eating.
- stand up and walk around the room.
- take small sips of fizzy drink.
- If the blockage persists, contact your doctor or local hospital.
If you have persistent abdominal or chest pain, fever, or bleeding after the procedure, you must then seek urgent advice from the Endoscopy Department between 09:00 and 17:30 (01908 996 460) Monday to Saturday.
Outside these hours, please call a nurse on Ward 22 (01908 996 455) for advice or go to your nearest A&E department.
If you have a cancer, you should already have a contact number for your Nurse Specialist. If not, please contact the Upper Gastro-Intestinal (UGI) Nurse on 01908-660033 and ask switchboard to Bleep 1785.
