Gastroscopy
Please note, this page is printable by selecting the normal print options on your computer.
You have been advised by your GP or hospital doctor to have an investigation known as a Gastroscopy.
This procedure requires your formal consent. This booklet has been written to enable you to make an informed decision in relation to agreeing to the investigation. You will be required to sign a consent form on the day of the procedure, which is a legal document, therefore please read this booklet carefully beforehand.
If you are unable to keep your appointment, please notify the endoscopy unit as soon as possible. This will enable staff to give your appointment to someone else and to re-arrange another date and time for you.
You need to understand all the information, including the possibility of complications. There will be the opportunity to speak to a health care professional about anything that you do not understand on the day of the procedure before you sign the consent form.
What is a Gastroscopy?
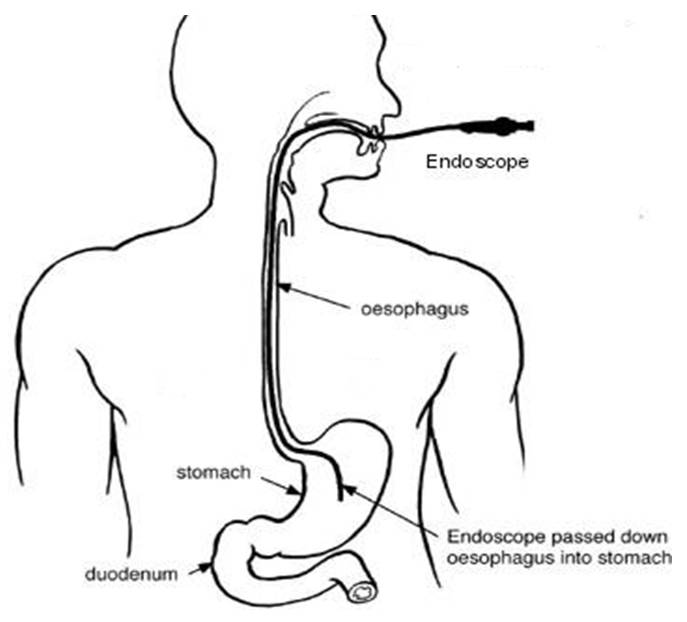
A Gastroscopy (which is also sometimes called an Upper Gastro-Intestinal endoscopy) involves putting a tube through the mouth into the oesophagus (gullet), down through the stomach and into the first part of the intestine (duodenum). By doing this the endoscopist can examine the upper digestive tract to detect any abnormality. Commonly found abnormalities are inflammation, hiatus hernia and ulcers. During the procedure, the endoscopist may take some samples (biopsies). This is a routine procedure which is not painful. The samples will be looked at under the microscope to help diagnosis and these will be retained by the pathology unit. Photographs may be taken and retained in your case notes.
Occasionally, treatment is required which can also be performed through the endoscope. This may involve treating any bleeding vessels or ulcers. Sometimes, there may be a narrowed area in the oesophagus which needs to be dilatated (stretched). These procedures will only be done if you have already given your permission and were discussed with you beforehand.
Are there any alternatives to a gastroscopy?
Your doctor has recommended a gastroscopy as it is the best way of diagnosing most problems with the upper digestive system. A barium meal is an x-ray test of the upper digestive system. This test is not as accurate as an upper GI endoscopy, and if your doctor finds a problem you may still need an upper GI endoscopy to perform biopsies. A urea breath test can be used to detect bacteria (helicobacter pylori) that can cause stomach ulcers.
How do I prepare?
To get a clear view of the oesophagus and stomach it is important that the stomach is empty. Please do not eat or drink anything for at least 6 hours before the procedure.
What about my medication?
Routine Medication: If you are on any medication, especially blood pressure tablets, you should take these with a sip of water first thing in the morning.
Diabetes: If you have diabetes and control this with insulin or tablets, please ensure that the Endoscopy Unit is aware so that your procedure can be booked for the beginning of the list. You will need to stop your diabetes medication during your “Nil by Mouth” phase. Your usual medication can be recommenced after the procedure once you are eating again. You may want to bring a sandwich with you to eat after the procedure with your usual diabetes medication.
If you have any further concerns, please contact your diabetic specialist nurse well in advance of the procedure for advice.
Anticoagulants/ Antiplatelets: If you are taking blood-thinning medicines, such as Warfarin, Dabigatran, Heparin, Dalteparin, Apixaban, Clopidogrel, the dose of these may need to be altered or stopped before your procedure. You may also need to have blood tests before your procedure. If the referring doctor did not give you instructions, you may be referred to the bridging clinic for advice on stopping your medication. If this is required, this will be arranged for you by the referring clinician or the endoscopy booking coordinator.
What to bring with you?
Along with your appointment letter you will have received a health questionnaire. Please complete it and bring it with you. You will also find enclosed a copy of your consent form; please read this carefully but do not sign it. This is just an example for you to read carefully prior to your appointment. The endoscopist will meet with you prior to your endoscopy to discuss what is going to happen, any risks and any serious or common side effects. At this point you will be given the opportunity to ask any questions and then you will sign the ‘actual’ consent form.
After your procedure you will be offered a choice of hot drink and biscuits. If you have any allergies/ intolerance, you might want to bring a snack as we are unable to cater for all dietary requirements.
How long will I be in the Endoscopy unit?
You should expect to be in the unit for approximately 2-3 hours. Please note that the time of your appointment is not the time that the procedure will be performed. How long you will be in the unit will depend on how quickly you recover from the procedure, the sedation you may have had and on how busy the unit is. The unit also looks after emergencies, and these can sometimes take priority over outpatient procedures.
You should be kept informed of any delays, but if you have any questions or concerns, please ask a member of the staff.
What happens when I arrive?
After checking in at reception, a qualified nurse will welcome you and take you to the admissions area where you will have a brief medical assessment. Please note that the endoscopy unit operates a same sex environment and your relative may not be able to accompany you past the waiting area unless there are exceptional circumstances. In the admission room, you will be asked some questions regarding your medical and surgical history to confirm that you are fit to undergo the procedure and about your arrangements for getting home. The nurse will make sure that you understand the procedure and discuss any questions you may have.
Your blood pressure, heart rate, respiration and oxygen levels will be recorded. If you have diabetes, your blood sugar level will also be checked and recorded. If you wear spectacles or dentures you will be asked to remove them when you enter the procedure room. All your belongings will be kept with you during your procedure to prevent anything being lost. You are advised to leave your valuables at home as we do not accept responsibility for them.
Many people decide to have a gastroscopy just with a local anaesthetic throat spray to make the throat numb. However, some need a little bit more help to keep them relaxed. If you have decided that you want sedation, which will be given later, the nurse will insert a cannula (a small plastic tube) into a vein in your hand or arm.
Sedation Options
You can decide to have your gastroscopy without sedation.
You can choose to have an intravenous sedative (usually Midazolam) and/or a painkiller (usually Pethidine or Fentanyl) which will be administered through an IV cannula (a plastic tube) inserted in a vein in your arm/hand. This will make you lightly drowsy and relaxed, but not make you go to sleep like a general anaesthetic. You will still hear what is said to you and therefore, will be able to carry out simple instructions during the procedure. Some people do not remember anything about the procedure once the effects have worn off.
Whilst you are sedated, we will monitor your breathing, respiration, and pulse rate via a finger probe, so that any changes can be recorded and dealt with accordingly. You will also be given some oxygen via a nasal sponge into your nostril. Your blood pressure may also be checked and recorded.
If you are having sedation, you must arrange for a responsible adult to collect you and stay with you overnight. If you have not been able to make these arrangements, you will not be able to have the procedure with sedation. You should not drive, return to work, operate machinery, or drink alcohol for 24 hours after the procedure, nor should you make any important decisions. The reason for this is that the sedation may, even though you may feel perfectly normal, still be in the body and may impair your judgement.
The gastroscopy procedure
After signing your consent form in the admission area, you will be escorted to the procedure room, you will be introduced to the team and a verbal safety checklist (called “WHO”) will be done.
Your throat will be made numb by using the local anaesthetic spray; you will then be asked to lie on your left side. A “probe” will be placed on your finger which can read your pulse and the amount of oxygen in your body (pulse oximeter). If you are having intravenous sedation, oxygen will be given, usually via a sponge which is placed into one of your nostrils. A mouth guard is placed lightly between your teeth. During the test, photographs may be taken if appropriate.
The procedure should take about 15 minutes.
Milton Keynes University Hospital is a teaching hospital and there may be a student and/or a trainee present in the room, or a supervised trainee may be doing your procedure. If you have any concerns or objections, please contact the Endoscopy Unit prior to your test, or make the nurse admitting you aware of this.
Aftercare
After the procedure, you will remain in the Endoscopy Unit for about 40 minutes if sedated. This is to enable the numb feeling in your throat to wear off. You may feel some abdominal bloating due to the air which will have been pumped into your stomach during the procedure.
When do I know the result?
Usually, the doctor or nurse will be able to tell you the results straight after the test, or if you have been sedated, when you are discharged. However, if a sample (biopsy) has been taken for examination, the results may take several weeks. Details of results and any necessary treatment should be discussed with your general practitioner (GP) or the consultant who referred you to have the test. A nurse will discharge you, discuss any aftercare and follow up needed and answer any questions you may have.
Before leaving you should receive written information on your procedure and a copy of the consent form.
If you are having sedation, the person collecting you must come to the unit to collect you. We advise that they park in the multi-storey car park or car park C before reporting to the Unit.
Are there any risks or complications?
A Gastroscopy has some risks associated with it. These occur infrequently, but we wish to draw your attention to them in order to help you make your decision. The doctor or specialist nurse who has requested the test will have considered this already. The risks must be compared with the benefit of having the procedure carried out.
The possible complications of gastroscopy are listed below. Any numbers which relate to risk are from studies of patients who have had this procedure. Your doctor will tell you if the risk of complications is higher or lower for you.
- Sore throat, which gets better quickly.
- Allergic reaction to equipment, materials, or sedative. The endoscopy team is trained to detect and treat any reaction that may happen. Let the admitting nurse and endoscopist know if you have any allergies or you have reacted to any drugs or tests in the past
- Breathing difficulties or heart irregularities, as a result of reaction to sedation or inhaling secretions such as saliva. To help prevent this from happening, your respiration and oxygen levels will be monitored, and a suction device will be used to clear any secretions. Rarely, a heart attack or stroke (loss of brain function resulting from an interruption of the blood supply to the brain) can happen if you have serious medical problems.
- Aspirating fluid in airway (minor risk)
- Perforation – making a hole in the oesophagus, stomach, or duodenum (risk: 1 in 10,000). The risk is higher if there are any abnormal narrowing (stricture) which is stretched (dilated) – 2-5 in every 100 procedures. If a hole occurs, you will need to be admitted to hospital for further treatment which may include surgery.
- Damage to teeth and bridgework. The nurse will place a plastic mouthpiece in your mouth to help protect your teeth. Let the endoscopist and nurse know if you have any loose teeth or dentures.
- Bleeding from biopsy site or from minor damage caused by the endoscope (risk: less than 1 in 1,000 procedures). This usually stops on its own.
- Incomplete procedure. This can happen due to a technical difficulty, food or blockage in the upper digestive system, complications during the procedure, or discomfort. Your doctor may recommend another endoscopy or a different test such as barium meal.
- Sedation. This can occasionally cause problems with breathing, heart rate and blood pressure. If these problems do occur, they are usually short lived. Careful monitoring by the endoscopy team ensures that any potential problems can be identified and treated quickly. Older patients and those with significant health problems, such as breathing difficulties due to a bad chest, may be assessed by a doctor or specialist nurse before having the procedure.
- Complications can happen. Some of these can be serious and can even cause death (risk: 1 in 25,000).
You should discuss these possible complications with your doctor if there is anything you do not understand.
What to do if you feel unwell once at home
If you have persistent abdominal or chest pain, fever, or bleeding after the procedure, you must then seek urgent advice from the Endoscopy Department between 09:00 and 17:30 (01908 996 460) Monday to Saturday.
Outside these hours, please call a nurse on Ward 22 (01908 996 455) for advice or go to your nearest A&E department.
