Fractured Neck of Femur
Please note, this page is printable by selecting the normal print options on your computer.
Information for patients
This booklet aims to help you understand what is happening during your stay in hospital. It explains some of the things that may happen while you are with us and why.
CONTENTS:
Introduction
What Matters to Me?
What Is a Hip Fracture?
Why Do I Need Surgery?
Types of Surgery
What Are the Benefits of Surgery?
What Are the Risks of Surgery?
National Hip Fracture Database
Before the Operation: What to Expect
Anaesthetics
The Team Caring for You
After the Operation
Wound Management
Medication
Pain Relief
Bone Health
Nutrition and Diet
Rehabilitation
Introduction to Mobility Aids
Advice for Activities of Daily Living
Exercises
Stage 1 (Bed Exercises)
Stage 2 (Seated Exercises)
Stage 3 (Standing Hip Exercises)
Stage 4
Technique for Stairs and Steps
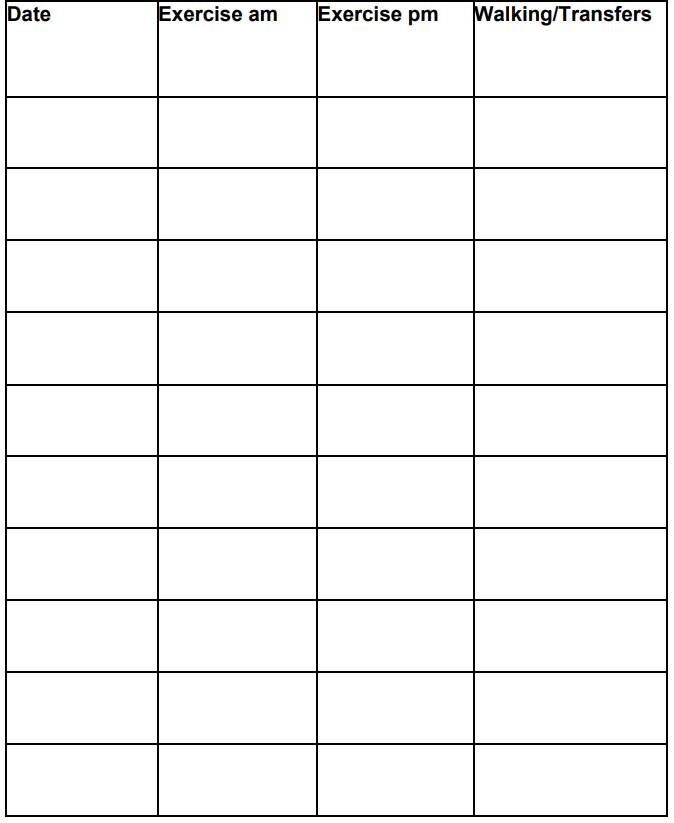
Exercise Log
Discharge from Hospital
Discharge Destination
Onward Referrals
Reablement
Physiotherapy
Falls Team
District Nurses
ASCAT
The Frailty Hub
Useful Numbers
PALS (Patient, Advice and Liaison Service)
INTRODUCTION
This booklet aims to help you and your relatives/ carers understand what is happening during your stay in hospital. It explains some of the things that may happen whilst you are with us and why. It also gives information about your discharge and ongoing rehabilitation. This includes education and advice on how to manage your condition and aid your recovery. Everyone is different. Therefore, some parts of this booklet may apply to you more than others. Your care and treatment may be slightly different to what is described but most of it will be similar. Please read the contents of this booklet and ask any members of our team your questions at any time.
WHAT MATTERS TO ME
Please try to fill in this section yourself or with the aid of carers/ relatives as early as possible.
I enjoy………
I would like to return to……..
I mobilise using ……
What else matters to me ……
WHAT IS A HIP FRACTURE?
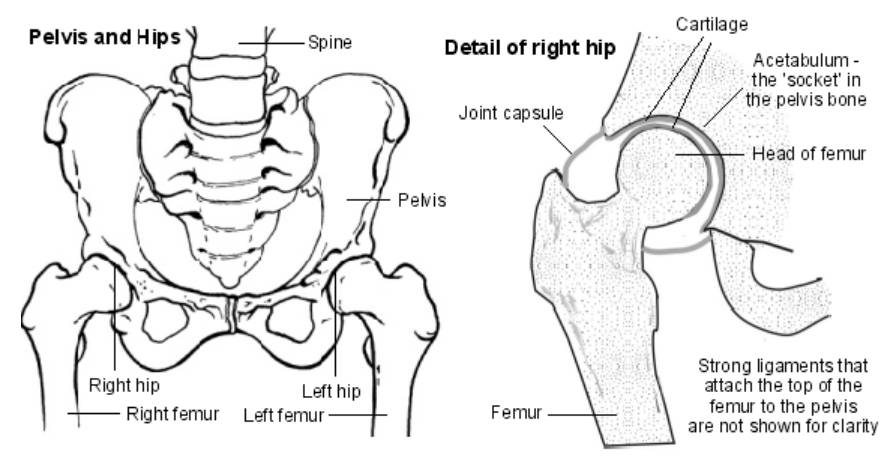
A neck of femur fracture is another term used to describe a broken hip. It is a very common injury, which mainly affects people over the age of 65. Around 75, 000 hip fractures are treated each year in the UK, and it is one of the most common reasons for being admitted to an Orthopaedic ward. Your hip is a ball and socket joint that sits between your pelvis (the acetabulum) and your thigh bone (the femur). A hip fracture is a break at the top of your femur. The type of operation you have will depend mainly on which part of the femur is fractured.
This is a serious injury, although the outcome for most patients, is good, the fracture alone is associated with causing high rates of illness and in the frail and elderly possibly even death within the first month (with or without surgery). The estimated risk of death for patients having an emergency operation for hip fracture is 10%. 1 in 10 patients die within 1 month. A person’s outcome will depend on how healthy they are prior to the injury.
WHY DO I NEED SURGERY?
We almost always recommend that you have an operation in order to fix the fracture. We aim to do it as soon as possible within our capacity. The earlier we fix your bone, the better your recovery in the longer term. In some cases, it may be best to treat the fracture without an operation. This would be discussed with you or your relatives and carers if the surgeon deems it the most appropriate course of treatment.
TYPES OF SURGERY
The type of surgery you will have will depend on the severity of the fracture and the part of the femur which is affected.
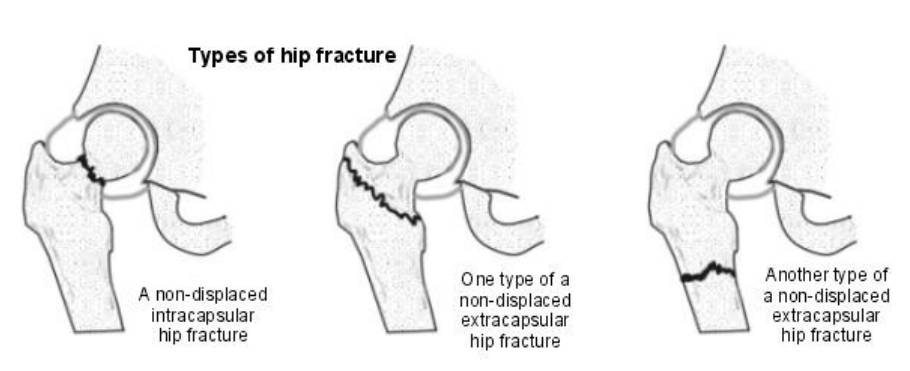
The most common hip fractures affect the head and neck of the femur. Usually this will be a displaced fracture, meaning the bones break and move out of place. In this case we replace the head of the femur. This can be done in one of two ways:
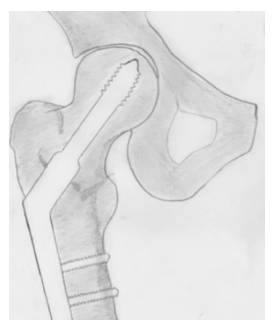
1. Hip Hemi-arthroplasty – replacing just the ball
2. Total Hip replacement – replacing the ball and the socket.
In both these operations, we remove the broken part of the femur containing the head (ball), replace it with a metal head, attached to a stem which we insert into your femur. This is usually with special cement, so the stem holds well inside the bone. In a total hip replacement, we also replace the socket (acetabulum). The type of operation you have will be dependent on your level of mobility and current health status. A total hip replacement is a bigger operation that national guidelines advise us to offer only to people who need little assistance with outdoor mobility, who have a good understanding of the rehabilitation process and have less co-morbidities.
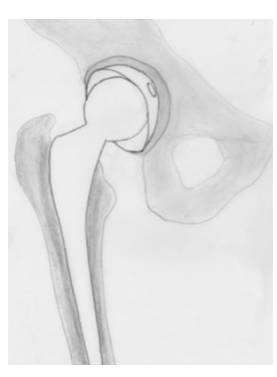
A total hip replacement
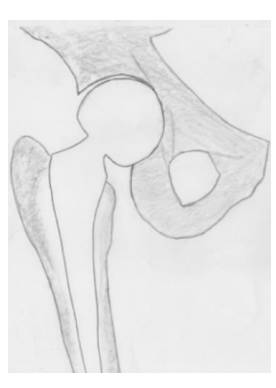
A Hip Hemi Arthroplasty
TYPES OF SURGERY:
If the fracture is below the level of the neck and there is low risk of disruption of the blood flow to the head of femur, surgery would involve stabilising the head. This can be done in one of two ways:
1. DHS (Dynamic Hip Screw) fixation
2. Intramedullary nail (IM Nail) fixation
As the fracture is below the neck of femur, nothing needs to be replaced. This can be fixed using a large screw or plate. A Dynamic Hip Screw involves insertion of a large screw into the head of
the femur with a plate on the outside of the femur, which aims to allow minimal movement by bringing the bone together to encourage healing. This is further benefitted through early weight bearing. Sometimes when the fracture is lower in the femur, a long metal rod is inserted into the femur instead. This will be fixed at the hip and the knee and is called an Intramedullary Nail (IM Nail). With this type of fixation, it is important to monitor your knee range of movement to avoid it becoming stiff.
DHS Fixation
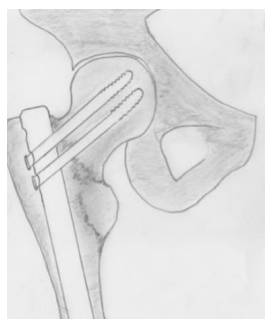
IM Nail Fixation
WHAT ARE THE BENEFITS OF SURGERY?
The idea of early fixation is to:
• Enable early mobilisation. This will allow you to stand, walk and put weight through your injured leg again day 1 after the operation.
• Relieve pain and discomfort. After the operation, you will have post-operative pain, which is normal, but your acute fracture pain will be relieved.
WHAT ARE THE RISKS OF SURGERY?
Listed here are the main risks involved with having these operations. Some of these are more common than others. As everyone is different, we will discuss individual risks with you and your relatives/carers.
- Wound Infection: There is a small risk of infection at the wound site. A dressing will keep it covered and clean, and your wound will be monitored for signs of infection whilst in hospital.
- Bleeding: There is a small risk of bleeding during the operation; therefore, you may need a blood transfusion if you lose blood either during or after the surgery. This will be monitored with a blood test.
- Thrombosis (Blood Clots): There is an increased risk of blood clots following your hip fracture as your mobility will be decreased. You will be offered blood thinning injections every day to reduce this risk.
- Dislocation: There is a very low risk of dislocation following your surgery. This is when the head (ball) of the hip replacement comes out of the hip socket.
- Delirium (Confusion): It is common to experience a temporary period of confusion whilst in hospital which may be referred to as delirium. There are a number of different symptoms, and it affects everybody differently. You may feel more disorientated than normal, or find it hard to remember things, you may feel agitated or hyperactive, or you may become more sleepy than usual. We will check you for subtle and early signs of this type of confusion. Common causes include constipation, infections, pain, new medications, dehydration, or simply being in a different environment.
- Delirium is only temporary, and you usually recover quickly. Relatives can help by visiting and informing our staff about you, your personality and your likes and dislikes so we can try and put you at ease during this time of confusion.
- Chest Infection: This is a risk following surgery and if you have been less mobile in bed. This is because your lungs cannot expand as much when lying. If this is diagnosed, you may need a course of antibiotics or chest physiotherapy to help treat this.
- Pressure Sores: You are at greater risk of developing pressure sores if you remain in the same position for a prolonged period. You will routinely be put on a pressure relieving mattress and the staff will check your skin integrity on a regular basis whilst in hospital.
NATIONAL HIP FRACTURE DATABASE:
A hip fracture is a common injury and caring for patients with a hip fracture is an important part of the work of the NHS. This hospital takes part in the National Hip Fracture Database (NHFD),
which has been set up to improve the care of patients who have broken a hip. Information gathered about care in hospital and about recovery afterwards enables us to measure the quality of that care and helps us to improve the services we provide. Reports based on NHFD data are made to our clinical staff to assist them in improving care here. The NHFD national reports show how
different hospitals compare, thus helping to improve standards of care nationally. So, information about your care and progress is important, and will be collected during your hospital stay. And, because your progress after you leave hospital matters to us, you may be contacted later about how you are getting on.
All information collected is confidential, and no information is ever made public about you or about any other patient. All NHFD information is stored, transferred, and analysed securely – both in this hospital and within the national database – in keeping with provisions of the Data Protection Act (1998). Participation is, of course, voluntary; and you are free, if you wish, not to take part – tell your Doctor if you do not wish to participate. However, the more people that take part, the more helpful NHFD will be in improving care. NHFD is supported by the National Clinical Audit Support Programme, a division of the Information Centre for Health and Social Care.

BEFORE THE OPERATION:
What to expect from admission to surgery?
Emergency Department:
You will be reviewed by the Emergency Department to assess your injuries. This will be completed through several investigations.
Hip X-Ray:
An X-ray allows Doctors to confirm that your bone is broken. Sometimes it can be difficult to see a small fracture on an X-ray image and further imaging may be required.
Chest X-ray:
A chest X-ray is often completed as a precaution to check for infection which may have contributed to your fall. It can then be used to plan the safest anaesthetic option for your surgery.
Electrocardiogram (ECG):
This shows us how well your heart is working. It may be completed as a precaution to rule out a reason for your fall.
Blood Tests:
Your bloods will be taken to review your blood levels. If anything is outside of normal ranges, then this can be treated prior to surgery.
Pain Relief:
Sufficient pain relief should be offered to you upon admission to hospital.
Following these investigations, you will be reviewed by an Orthopaedic Doctor and transferred from the Emergency Department to the appropriate ward. Your time of admission, your readiness for surgery and other scheduled operations will impact when you go for surgery. This will be explained to you and your relatives/carers by the Doctor. Once it is decided that you require an operation, the orthopaedic Consultant will come and see you to explain the procedure and answer any questions you may have. We will then ask you to sign a consent form and discuss the risks and benefits. This form must be completed by law prior to completing the operation. You can eat and drink up to six hours before the operation and drink clear fluids up to two hours before. At this time, we can give you fluids through a drip line if they are needed.
ANASETHETICS:
There are several types of anaesthesia with different benefits and risks. You may have more than one and the choice will depend upon assessment by an anaesthetist, who will take into consideration the type of surgery you are having and your past medical history. Below is the list of different types:
General Anaesthesia:
This is where you will be completely asleep during the operation. You are given medication through a drip line in to your vein, usually in your arm and/or medication that you can breathe in, before and while you are having surgery.
Neuraxial Block
This puts local anaesthetic around the nerves supplying your hip, high up as they leave your spine. You are either given an injection into your spine or as an epidural. This keeps you comfortable throughout surgery. You shall be awake with this option, but under sedation, during the operation.
Regional Nerve Block
This puts local anaesthetic directly around the nerves in the hip. A regional nerve block keeps you comfortable throughout surgery. You will be awake, but under sedation, during the operation.
THE TEAM CARING FOR YOU:
Orthopaedic Consultant:
The consultant will be the doctor that completes your surgery.
SHO Doctors:
The ward-based doctors will look after you on a daily basis and will coordinate information of your medical needs.
Nurses and Healthcare Assistants: Based on the ward and administer medications prescribed by doctor, support with personal cares, toileting and aid in your recovery following surgery.
Orthogeritrician: Consultant who specialises in the care of the elderly following Orthopaedic Surgery. They will work alongside the orthopaedic doctors on the ward.
Anaesthetist: Helps the surgical team to plan and carry out a safe operation.
Physiotherapist: Support you in mobilising out of bed following your operation, issue appropriate mobility aids, provide advice and education on rehabilitation and continue to review you throughout your inpatient stay.
Occupational Therapist: Provide you with equipment and techniques to aid your everyday routine so you can be as independent as possible. Liaise with family members/carers and discharge team to ensure you have a safe discharge destination.
Dietician: Assess if you are at risk of malnutrition and provide you with nutritional support if deemed appropriate.
Discharge Officer: Liaise with multi-disciplinary team to make onward referrals to enable safe discharge.
Trauma Coordinator: Co-ordinates the work of all multi-disciplinary teams involved in your care to ensure that you have a smooth journey in hospital and receive the best care we can offer.
Fragility Advance Nurse Practitioner: Identify patients, who have sustained a Fragility fracture, assessing and initiating treatment for those with osteoporosis. In accordance with NICE, Royal Osteoporosis Society Guidelines.
Pharmacist: Review your medications when you are admitted to hospital, throughout your admission and on discharge.
AFTER THE OPERATION:
When you wake up from your operation you will be on the recovery ward where we can observe you more closely straight after surgery. You will stay there until you are well enough to return to the Orthopaedic ward.
WOUND MANAGEMENT:
Metal clips are usually used to hold your wound together. These stay in place until your wound looks as if it is healing well with no signs of infection. The clips are usually taken out 10-14 days post-operatively. This can be completed on the ward if you are still in hospital, or a nurse can come and visit you in the community. This will be arranged via the ward prior to your discharge.
PAIN RELIEF:
When in hospital, you may be started on some new medication. The Doctors and Pharmacists will explain to you what they are for and how to take them. When you leave hospital, we will give you two weeks supply of all medication and we will also send a letter to your GP so they can continue to give you repeat prescriptions. Alongside other medications, you will be given two weeks supply of pain relief you have been taking whilst in hospital. If you require a repeat prescription or additional pain relief if you pain is not being controlled, please speak to your GP. It is important you keep your pain well controlled in order to allow you to progress your mobility.
BONE HEALTH:
As you have broken your hip, you are at high risk of Osteoporosis, a condition which makes your bones weaker. Broken bones are often the first sign of this condition, so we will assess you while you are in hospital. This involves having some blood tests and asking questions about your lifestyle and any other medical problems. If needed we can then give you a personal management plan, which may include taking medication to help strengthen your bones. You may also be referred for a scan called a DEXA (Dual Energy X-ray Absorptiometry), which will measure the strength of your bones. This will happen as an outpatient once you have left hospital. You will be followed up by the Fragility Nurse (either in clinic or over the telephone) 10-12 weeks after discharge. This will give us a chance to educate you, follow up any medication started and monitor your progress.
NUTRITION AND DIET:
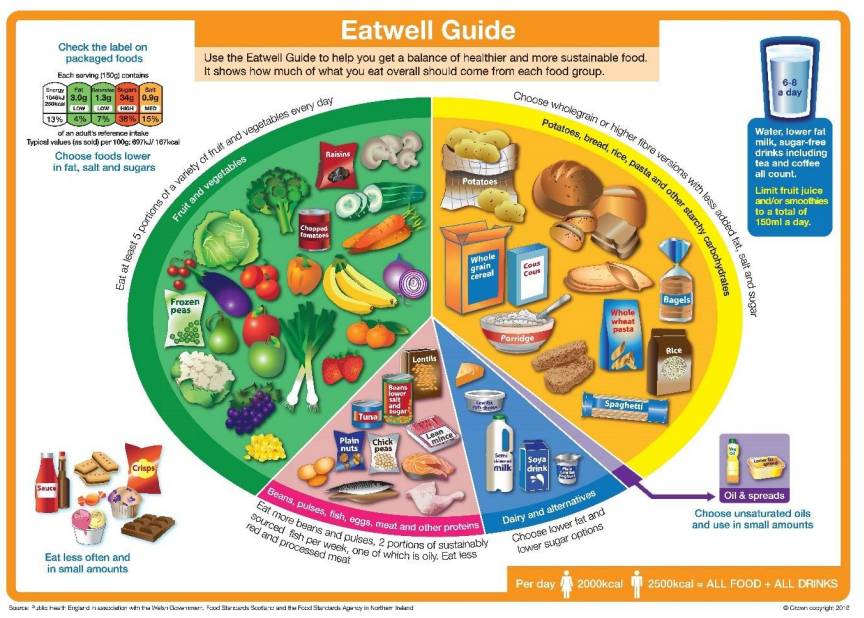
Following your surgery, it is important to ensure that you are eating well to provide your body with the nutrients it needs to aid recovery Aim to consume a diet which is balanced, based on the eat well guide:
• Aim to eat at least 5 portions of a variety of fruit and veg each day. Choose from fresh, frozen, tinned, dried or juiced.
• Starchy food should make up just over a third of the food we eat. Choose higher fibre wholegrain varieties, such as wholewheat pasta and brown rice, or simply leave skins on potatoes.
• Milk, cheese, yoghurt and fromage frais are good sources of protein and some vitamins, and they’re also an important source of calcium, which helps keep our bones healthy.
• Meat, beans, pulses, fish, eggs, meat are good sources of protein, vitamins and minerals. Pulses, such as beans, peas and lentils, are lower in fat and higher in fibre and protein, too.
• Unsaturated fats are healthier fats and include vegetable, rapeseed, olive and sunflower oils. Remember all types of fat are high in energy and should be eaten sparingly.
• Eat foods high in fat, salt, and sugar less often and in small amounts- however if your appetite is low or you struggle to maintain a healthy weight, these can be consumed in higher amounts- speak to a dietitian for more advice on this. Those who have had a neck of femur injury may be at risk of malnutrition due to reduced appetite, frailty, and poor dietary intake during, or before admission.
If your appetite is low, consider the following tips:
• Always have breakfast –you will find you will eat better for the rest of the day.
• Try eating little and often. Aim for 3 small meals and 2-3 snacks and/or milky drinks.
• Drink towards the end of your meal or after so that you do not spoil your appetite.
• Use one pint of full cream milk daily, by itself or in drinks or puddings (if you are lactose intolerant or vegan, try soya milk or rice milk instead of cows’ or goats’ milk).
• Have a pudding once or twice a day e.g. fruit pie and ice cream, sponge with custard or cream, slice of cake, ready prepared dessert or milk puddings. Why not have one as a snack? Consider at least two ‘between meals’ snacks, examples of high calorie snacks include:
• 2 small pieces (match box size) of cheese and an apple or bunch of grapes
• Medium Cornish pasty
• Hummus and pitta bread
• Bowl of cereal and fortified milk (see below)
• Slice of fruit cake and cheese
• 3x medium size samosas
• Croissant with cheese
Try Enriched Milk: Add 4 tablespoons of dried milk to 1 pint of whole milk to double to calorie and protein content, this allows you to consume the same volume of milk but more nourishment.
• To make jelly, by dissolving the jelly in half the recommended water and once it has cooled a little use the fortified milk to make the jelly up to the right amount.
• To make up a cuppa soup, make the fortified milk as above, follow the directions on the packet but substitute the hot water for fortified milk.
• In puddings, sauces, custards, jelly, cuppa soup, and breakfast cereal.
Try fortifying your food:
• Add grated cheese, milk powder, butter/margarine, or cream to soups, sauces, mashed potatoes.
• Add extra butter or margarine to vegetables, potatoes, scrambled egg and bread.
• Add extra sugar / honey to hot milk, tea, coffee, herbal tea, breakfast cereal.
• Add sugar, honey, peanut butter or jam to milk pudding, breakfast cereal, yoghurt.
If you find your appetite continues to be poor, or you are struggling to regain lost weight, please alert your GP, or a dietitian.
REHABILIATION:
Following your operation, your rehabilitation starts straight away. The aim of fixing broken hips is to enable you to put weight through the injured leg and start using your hip again the very next day. On the first day post operation a Physiotherapist will come to assess you, which will initially include checking your sensation and muscle power. It will be expected that you mobilise out of bed on your first day and the Physiotherapy team will assist you with this using different types of equipment.
The Occupational Therapy team will review you the day of or day after your operation. They will ask lots of questions about your home environment and how you were managing before this injury. They may also contact your relatives/carers to gather this information if deemed appropriate. The aim is to establish your baseline which allows them to start to plan a safe and appropriate discharge. Therapy input should be taking place on a daily basis during your inpatient stay. However, your rehabilitation should not just be with Physiotherapists. There are exercises in this booklet and you will be advised which ones you should aim to complete throughout the day. It is important to get out of bed on a daily basis and if you have been told you are safe to mobilise with the Nursing Staff, then you should be doing so as regularly as possible.
INTRODUCTION TO MOBILITY AIDS:
Below is a selection of transfer and mobility aids which you may use throughout your stay with us.
Sara Steady: This is a transfer aid which enables you to perch whilst transferring from bed to chair. This requires you to stand for paddles to be placed in behind you.
Re-turn: This is a transfer aid which enables you to be transferred whilst you maintain a safe stand. It has three bars which allow you to use your arms to stand.
High Roller: This is a mobility aid which allows you to lean through your arms to walk. It is height adjustable and has four wheels. Note you cannot be discharged home mobilising with this aid.
Zimmer Frame: This is an indoor mobility aid with two wheels and two stoppers. A caddy can be attached to the front of the frame to increase independence.
Gutter Frame: This is similar to a zimmer frame but allows greater weight bearing through arms due to forearm support.
Elbow Crutches: This is a more advanced mobility aid which can be used outdoors. They require a high level of balance, making them unsuitable for some people following their operation.
Outdoor Walkers: These are walkers that can be used safely outdoors. They have either three or four wheels. If this was deemed appropriate for you, it would be assessed in the community following discharge.
ADVICE FOR ACTIVITIES OF DAILY LIVING:
Washing
• Whilst your hip is healing you may find it difficult to access a bath.
• Therefore, if you do not have a walk-in shower or shower cubicle it may be more comfortable to have a strip-down wash.
• If you find it difficult to wash below your knees, you will either have to use a long-handled sponge or ask someone to do this for you.
• If you have a step into your shower cubicle, negotiate this using the way taught by your physiotherapist.
• If you have a seat in your shower, ensure it is a reasonable height, so it does not cause discomfort to your hip.
Dressing
Always dress your operated leg first and undress it last. Sit in a chair or on the bed; have all your clothing and dressing aids within easy reach. Place the hook of your long-handled shoehorn through the operated leg side of your underwear and hook the underwear to the shoehorn. Lower the long-handled shoehorn down the operated leg and feed underwear over your toes. Bring underwear up to knee level and then dress the un-operated leg in your normal manner, remembering not to bend forwards too far. You may also use the shoehorn or helping hand to dress this leg if required.
If wearing trousers, use the long-handled shoehorn or helping hand to lower your trousers onto the floor. Slip the trouser leg over your operated leg first, then do the same for your non-operated leg. If your trousers have belt loops, put the hook of the shoehorn through the loop and then lower the trousers to the floor. Pull your trousers and underwear above knee level before standing to
adjust clothes. If you wear braces, place these on your shoulders prior to standing. When undressing, remove your trousers/undergarments from the non-operated leg first, and reverse the above steps.
Toilet Transfers
When sitting down ensure that the height of the seat is both comfortable for your hip and enables you to sit down in a controlled manner. If you feel the height of your toilet is too low or you would need armrests/rails to push up from to achieve a controlled sit and stand, your Occupational Therapist can discuss and further assess for this.
Bed Transfers
A high, firm bed is recommended.
• Place yourself in a sitting position on the side of the bed.
• Using your upper body strength and leaning slightly backwards, slide your buttocks towards the pillow.
• Lift legs onto the bed.
• When getting out of bed, reverse above technique. It is advised to sleep on your back or unoperated side while your wound is healing.
Car Transfers
Use the front passenger seat. Have the seat as far back as possible and the backrest angled so that it is partially reclined.
• With passenger door open, back up to the car until you feel the seat against the back of your knees. Facing away from the car, before sitting, put your left hand on the top of the passenger seat for support and, with the door window fully open, grip the open door window frame with your right hand. Have someone hold the door to prevent it closing toward you.
• Gently lower yourself down, remembering to keep your operated leg extended. Lift yourself backwards, moving your bottom towards the driver’s seat. You may find this easier with a plastic bag on the seat to reduce any friction and aid in swivel. While you are leaning backwards, carefully lift your leg and slide into the car • If the car seat is low or slopes backwards, raise or level it out with a cushion.
• You must get into the car from road or drive level, not from the pavement.
Driving
• You will not be able to drive for a minimum of 6 weeks postoperatively. After this time, please ask your consultant for advice.
• You are advised to contact your insurance company to inform them of your surgery.
EXERCISES:
Do these exercises 3-4 times a day. Your Physiotherapist will advise you on which exercises to complete. Please note, there are a list of exercises here which are progressions. Do not attempt to complete these exercises unless advised and taught to do so by your Physiotherapist.
STAGE ONE (BED EXERCSIES):
Exercise 1
• Sitting or lying on your back
• Squeeze your buttocks together
• Hold each exercise for 5-10 seconds, relax then repeat x 10
Exercise 2
• Sit or lie with your legs straight out in front of you
• Move your ankles up and down
• Repeat x 10

Exercise 3
• Sit or lie with your legs straight out in front of you
• Push the back of your knee down towards the bed
• You should feel the muscle on the front of your thigh tighten
• Hold for a count of 5, relax then repeat x 10
Exercise 4
• Sit or lie with your legs straight out in front of you
• Slide the heel of your operated leg towards your bottom and allow your hip and knee to bend
• Slide your heel back down again, relax and repeat x 10

Exercise 3
• Sit or lie with your legs straight out in front of you
• Push the back of your knee down towards the bed
• You should feel the muscle on the front of your thigh tighten
• Hold for a count of 5, relax then repeat x 10
Exercise 4
• Sit or lie with your legs straight out in front of you
• Slide the heel of your operated leg towards your bottom and allow your hip and knee to bend
• Slide your heel back down again, relax and repeat x 10

STAGE TWO (SEATED EXERCISES):
Exercise 6
Marching on the Spot
• Try marching on the spot.
• Focus on small movements first and then move your knees higher as able.
• Repeat x10 on each leg.

Exercise 7
Knee Extension

• Straighten one leg out in front of you
• Make sure your toes stay pointed to the ceiling throughout
• Hold for 3-5 seconds and slowly lower leg back.
• Relax and repeat on other leg. Complete x10 on each leg.
Exercise 8
Seated Heel Raises and Toe Raises
• Leave your toes on the floor and raise your heels up and down.
• Then, leave your heels on the floor and raise your toes up and down.
• Relax and repeat x10 on each leg

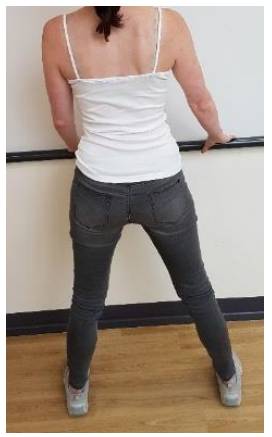
STAGE THREE (STANDING HIP EXERCISES):
Exercise 9
• Stand with your hands supported on a table or high-backed chair. Lift the knee of your operated leg towards your chest, therefore bending your hip.
• Lower your foot to the floor, relax & repeat x 10
• Change to the unoperated leg and repeat

Exercise 10
• Stand with your hands supported on a table or high-backed chair
• Keep your body straight and upright throughout the exercise
• Move your operated leg backwards as far as possible
• Return to the starting position
• Change to the unoperated leg and repeat x 10
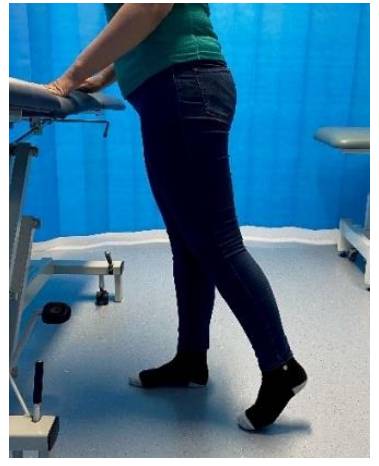
Exercise 11
• Stand with your hands supported on a table or high-backed chair
• Keep your body straight and upright throughout the exercise
• Move your operated leg out to the side as far as possible
• Return to the starting position
• Relax and repeat x 10
• Change to the unoperated leg and repeat x 10

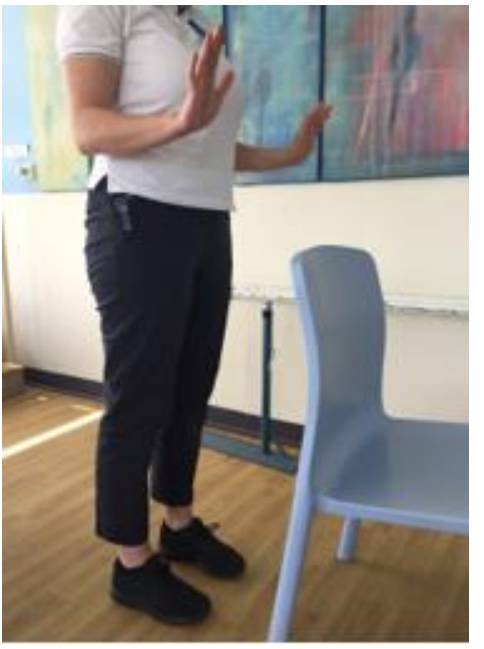
Exercise 12 Unsupported standing
▪ Stand in front of a stable surface, like a table or a frame.
▪ With feet shoulder width apart, take your hands off the support.
▪ Aim to stand for 30 seconds unsupported.
If unable to, do as long as you can and gradually increase.
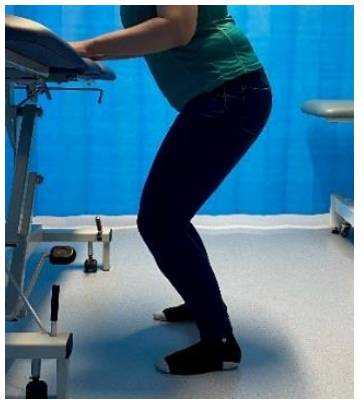
STAGE FOUR:
Exercise 13
Mini Squat
• Stand with your hands supported on a table or kitchen work surface.
• Slowly bend your knees. Make sure your knees do not move over your toes.
• Straighten knees slowly.
• Relax and repeat x 10.
Exercise 14
Bridging
• Lie on your back on the bed with knees bent.
• Lift your pelvis off the bed.
• Hold for 3-5 seconds and slowly lower back onto bed
• Relax and repeat x 10

Exercise 15
Side stepping
• Stand with your hands supported on a table or kitchen work surface
• Take a step to your right with your right leg, then close with your left leg so that you are standing with your feet hip width apart
• Repeat this movement until you reach the end of your table/ kitchen work surface
• Repeat this process stepping to your left
• Relax and repeat x10
Exercise 16
Sit to stand
• Sit tall near the front of your chair
• Place your feet on the floor slightly underneath you
• Lean forward slightly keeping your back straight
• Squeeze your buttocks together then stand up (use your hands on the chair if required initially)
• Step back until your legs touch the chair
• Lean forward as you bend your knees, then slowly lower your bottom into the chair in a controlled fashion (use hands for balance if required initially)

TECHNIQUE FOR STAIRS AND STEPS:
Using crutches on stairs:
With no rail:
• Use 2 elbow crutches
• Hold them as you would for walking
With one rail:
• Use one elbow crutch and one rail/banister
• Then hold both crutches in one hand in a ‘T’ shape
With two rails:
• Use 2 rails/banisters
• Have someone who can carry your crutches.
Going up stairs:
1. Stand at the bottom facing upwards
2. Hold onto rails and/or crutches
3. Move good leg up one step first
4. Move affected leg up onto same step
5. Move crutch to same step and/or move hands up rail
6. This process is repeated until you reach the top

Going downstairs:
1. Stand at the top of the stairs facing down
2. Hold onto rail and/or crutches
3. Move crutches down one step and/or move hands down rail
4. Move affected leg down to the same step
5. Move good leg down onto the same step
6. This process is repeated until you reach the bottom

If you have a step either inside or to access your home use the same technique as above if using crutches and/or rails. If you are using a zimmer frame, follow the technique below:
Going up step:
1. Stand in front of the step facing up
2. Lift frame onto step, ensuring it is fully on the step before proceeding.
3. Step as close to step as possible
4. Move good leg onto step first
5. Move affected leg onto same step
Going down step:
1. Stand in front of step facing down
2. Lift frame from step to ground, ensuring it is fully on the ground before proceeding
3. Get as close to edge of step as possible
4. Move affected leg onto ground first
5. Move good leg onto ground
EXERCISE LOG:
Use the table below to log when you do your exercises. It is important that you manage to complete your exercises daily once discharged from hospital.
DISCHARGE FROM HOSPITAL:
How long you stay in hospital depends on many things such as your ability to walk again, your general health and any complications after surgery. As you improve with the therapists, they will continue to assess the best place for you to be managed. This may be to stay on the ward, to return home and receive therapy at home or to be referred for inpatient rehabilitation outside of the acute hospital. Your discharge destination will always be discussed with you and your family/carers, and a joint agreement will be made with you to deem what is most appropriate for your discharge.
DISCHARGE DESTINATION:
Inpatient Rehabilitation: There are two rehabilitation units within Milton Keynes, Windsor Intermediate Care Unit (WICU) and Waterhall. Both facilities are in Bletchley, Milton Keynes. If it is deemed you require a rehab bed, you will be advised which unit your bed is at based on capacity of each unit.
Recuperation Bed: If there are concerns that you may not manage going home from hospital then you may be referred for a recuperation bed in a residential setting. From here you will be continually assessed to determine your safety to return home.
Home: You may be able to return home from hospital. This may be withadditional care which can be organised in hospital.
OWNWARD REFERRALS:
The information below applies to patients that live within the Milton Keynes area or have a Milton Keynes GP. If you live outside of this area, you will be referred for similar services. The service can vary dependent on where you live but will be discussed with you prior to discharge.
REABLEMENT:
This is a short-term care package for approximately six weeks which is funded if it is deemed you require it. Carers will determine how often you require care calls, and this will be continually reassessed throughout the six weeks. If it is identified that you require more long-term care at home, assessments can be completed to implement the most appropriate care package for you.
PHYSIOTHERAPY:
You will be referred for follow-up Physiotherapy on discharge from hospital. Your level of mobility will determine which team you are referred to. If it is identified that you require therapy input on day of discharge, you will be referred to Home First Therapy Team. This team offer short term therapy intervention at home to ensure you are safe. If you are safe for discharge home without immediate therapy needs, you will be referred to our in-house Orthopaedic Outreach Team. They will be in contact with you within two weeks of your discharge and they will work with you to achieve your goals and improve your mobility.
FALLS TEAM:
If the reason for your admission is due to a fall that is mechanical in nature, you should be referred to the falls prevention service that covers your local area. They can advise and support you with how to reduce your risk of falling again.
DISTRICT NURSES:
If it is deemed that you require district nurses to either check your wound or aid with medication you will be referred by the ward prior to discharge.
ASCAT:
If you feel you are struggling with personal care or feel you would benefit from an Occupational Therapy assessment at home, you can refer yourself to the Adult Social Care Access Team (ASCAT)
on 01908 253772. This is only for patients who live within the Milton Keynes area.
THE FRAILTY HUB:
The Integrated Community Support Remote Frailty Hub is a service ran by CNWL NHS Services in order to support frail patients in the community post hospital discharge. The service enables and supports people to live as independently as possible and manage their own lives to reduce unplanned services.
The Criteria:
• You must be 65 years of age or older, registered with a Milton Keynes GP and have 1 or more of the following:
• Be on 4 or more medications,
• Frequent, unplanned attendances to hospital (4 or more within 12 months),
• Have a Rockwood clinical frailty scale of 4 or above,
• Has a cognitive impairment or in need of psychological support,
• Experienced a recent change in circumstances and may benefit from strategies to reduce risk and improve health awareness,
• Have 2 or more health/ social care professionals involved resulting in the need to co-ordinate services,
• Would benefit from a comprehensive assessment to reduce risk and improve health awareness.
Self Refer:
• Telephone: 01908 724577
• Email: [email protected]
• Provide: Name, Address, DOB and the reason for your referral.

USEFUL NUMBERS:
Milton Keynes University Hospital: 01908 660033
Pharmacy Medication Information: 01908 995733
Trauma and Orthopaedics: 01908 997006
Orthopaedic Outreach Physiotherapy Team: 01908 995431
Home First Physiotherapy Team: 01908 724999
ASCAT: 01908 253772
Age UK: 01908 550700
Apetito (Meals on Wheels): 01908 217254
Red Cross (Wheelchair and Equipment hire): 01296 739300
Telecare (Pendant Alarm): 01908 222616
Wiltshire Farm Foods: 01525 242220
Silver Line (Befriending Service): 0800 4708 090
MK Carers: 01908 231703
PATIENT ADVICE AND LIASION SERVICE:
Patients, relatives and their carers sometimes need to turn to someone for on-the-spot help, advice and support or give feedback on their experience whilst in hospital.
PALS can help by:
Advising and supporting patients, their families, and carers:
• Listening to your feedback and ensuring it is used to improve services to our patients and the public
• Listening to your comments, compliments, concerns, and complaints
• Helping sort out problems quickly on your behalf
Contact:
Tel No: 01908 995954 or 01908 996222
E-Mail: [email protected]
Or write to us at:
PALS
Milton Keynes University Hospital NHS Foundation Trust
Oaks House, Standing Way, Eaglestone, Milton Keynes, MK6 5LD.
