Eating when you have an Oesophageal Stent
Please note, this page is printable by selecting the normal print options on your computer.
What is an Oesophageal Stent?
Figure 1 – Inserted stent
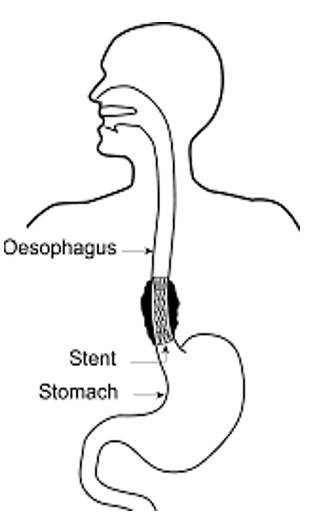
A stent (flexible mesh tube) is placed in the narrowed area of your oesophagus (gullet), where it gently expands to allow food and fluid to pass into the stomach more easily (figure 1). The stent is not as wide or as flexible as a normal oesophagus, so it is important to take care of which foods to eat to prevent the stent from blocking.
You will not be able to eat or drink for four hours after the procedure. Once the stent is confirmed in place, only clear fluids (water, squash, herbal or fruit teas, jelly, Ensure Juce, or beef extract drinks such as Bovril®) may be taken for the remainder of the day.
Once the doctor allows you to eat (usually the next day), aim to reintroduce food gradually, starting with liquid/puree foods, followed by soft foods (coded by a star on the hospital menu).
It is important that you:
Do:
|
Do Not:
|
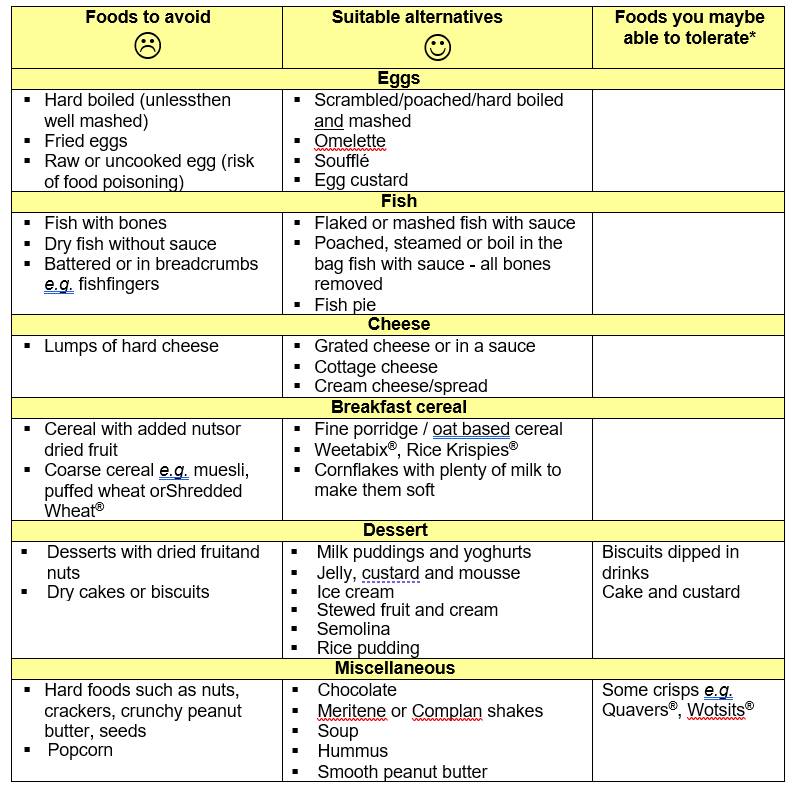
Over the following weeks, you will be able to increase the types and textures of foods that you can manage. Please see below for further guidance on the suitable food choices:
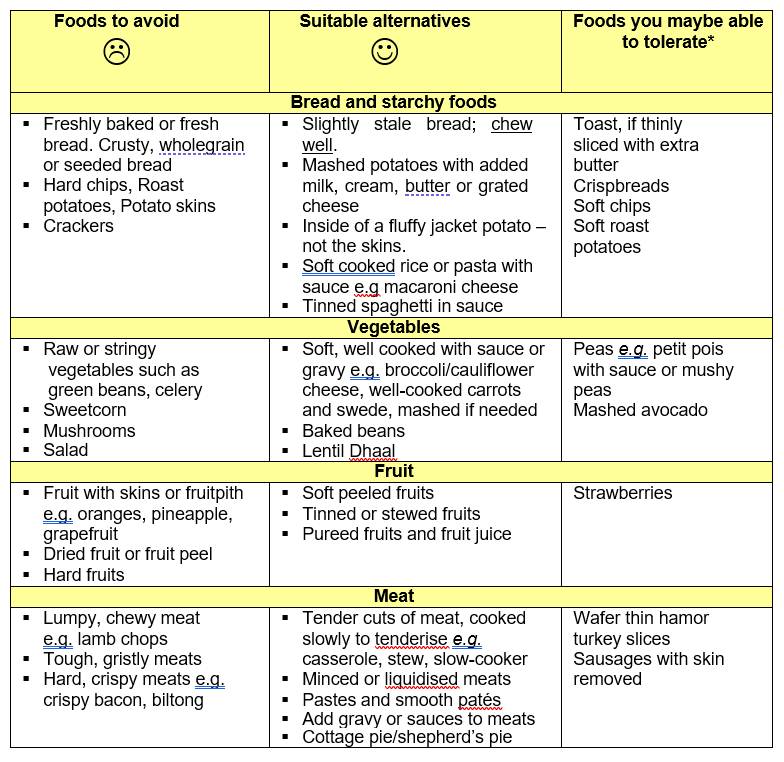
*Depending on the opening of the stent and how well food is chewed.
Remember to have frequent sips of fluid between and after meals to wash down your food. Fizzy drinks can cause symptoms of acid reflux. Warm water is a better option if you feel food is trapped in your stent.
How to maintain a balanced diet:
- Eat regularly – You may find that three small meals with snacks in between are easier to manage, especially if you have a small
- Try to include a range of different food to get all the nutrients you need, including:
- Suitable meats, fish, and pulses
- Dairy foods such as milk, yoghurt, and cheese, or fortified alternatives
- Starchy foods such as potatoes, pasta, rice, breakfast cereals, and bread
- Suitable fruits and vegetables (including tinned and juiced varieties)
- Drink 6-8 cups of fluid every
What to do if you are losing weight:
If you find you are losing weight unintentionally, try the following:
- Have a soft pudding after meals – eg sponge and custard, milk pudding, ice cream, creamy yoghurt, tapioca, or jelly.
- Enrich the foods you eat by adding butter to soft vegetables and mashed potato; adding grated cheese to scrambled eggs, omelettes and pasta dishes; adding cream, milk powder, or evaporated milk to hot drinks; or adding honey/jam to yoghurts and breakfast cereals.
- Have nourishing drinks such as hot milky drinks, full fat milk, milkshakes, fruit juice, and soups in between You could also buy fortified drinks from the supermarket/chemist such as Meritene® and Complan®.
- Ready Meals/Meals on wheels – If you find cooking is difficult or makes you tired, convenience foods can be useful. Try shop-bought ready meals or find a company who can deliver frozen ready meals to your house. Some of these produce soft or pureed ranges of foods. Ask a dietitian for more details.
- Visit your dentist if damaged/loose teeth or dentures are limiting the foods you can
If you would like more information on gaining weight, ask the Dietitian for the ‘Food First’ dietary leaflet. If you have been discharged from hospital, this information can also be obtained from your GP or specialist nurse.
If you have any queries regarding your diet, contact the Dietetic department on 01908 995387. The department can also be contacted through the Hospital’s main switchboard.
