Dietary Advice for Ulcerative Colitis
Please note, this page is printable by selecting the normal print options on your computer.
What is Ulcerative Colitis
Ulcerative Colitis (UC) is a form of Inflammatory Bowel Disease (IBD). IBD is a term used to cover a number of inflammatory conditions of the gastrointestinal tract. UC causes inflammation in the large bowel and can affect the rectum, part of, or the entire colon. If you have UC this diet sheet may help you.
Can diet help?
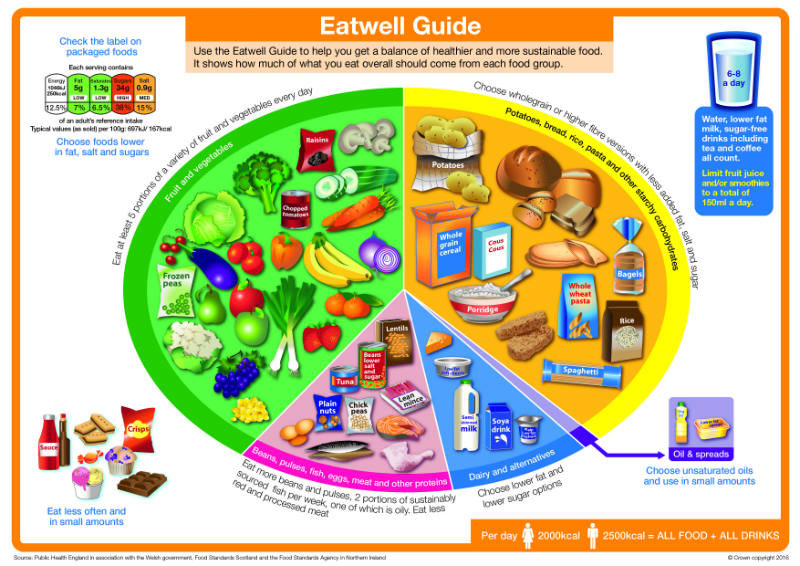
Diet is not a cause of UC; however diet can help to relieve symptoms such as diarrhoea during a flare up; and maintain good health including healthy bones. You may find as time goes by you begin to notice that certain foods aggravate your symptoms of UC and so they are best avoided. However, do not remove whole food groups as this could mean you lose some vital nutrients. The main food groups are demonstrated below in the ‘Eatwell Guide’.
What foods are beneficial for UC during a flare up?
Soluble Fibre – Dietary fibre can be categorised into two forms, soluble and insoluble. Soluble fibre is partially digested (broken down) in the large intestine to form a glue like substance, which helps to produce soft/formed stools, without causing inflammation. Examples of foods rich in soluble fibre are:
- Oats e.g. Porridge oats/Ready Brek ®, oatcakes
- The body of fruits and vegetables e.g. peeled apples and pears, tinned fruit, peeled root vegetables such as carrots, parsnips, turnip
What foods may worsen UC during a flare up?
Insoluble Fibre – This type of fibre may not be tolerated well as it speeds up bowel motions and can irritate the colon further as it travels through the gut. Examples of foods high in insoluble fibre are:
- Wholemeal or granary bread
- Wholemeal rice or pasta
- High fibre cereals e.g. Bran flakes®, Shredded Wheat®
- Sweetcorn, mushrooms, onions (especially raw), broccoli, cabbage, cauliflower
- Skins of fruits & vegetables e.g. Jacket potato skins, peppers, tomatoes, cherries, grapes, dried fruit.
- Nuts, seeds and popcorn.
Dairy foods
Some people find they are unable to tolerate the lactose found in dairy foods such as milk, cheese, yogurts especially during a flare up. If you do chose to avoid lactose it is important to continue to include sources of calcium in your diet to maintain bone health. Examples of lactose-free alternatives rich in calcium are:
- ‘Low Lacto’ or ‘Lactose Free’ milks and milk products.
- Soya, Rice or Oat milks fortified with calcium.
- Hard cheese rather than soft cheese may be better tolerated.
What foods may worsen UC during a flare up?
Spicy foods and fatty foods
Spicy foods and fatty foods may aggravate the colon during a flare up and possibly cause loose stools In order to maintain a healthy balanced diet it is important to reintroduce any excluded foods as tolerated, once your flare up is over.
What about Probiotics?
Probiotics are ‘friendly’ gut bacteria that are available in capsule, liquid (usually yoghurt drinks) and powder form. They are considered safe to take if you have UC and may have beneficial properties. They are used in management of pouchitis, but research into their use generally in UC is ongoing.
What about fish oils?
Fish oils that are rich in omega 3 fatty acids have been found to have an anti-inflammatory effect. However, there is currently no conclusive evidence whether they are beneficial to those suffering from UC.
Do I need multivitamin and mineral supplements or supplement drinks?
You should be able to get all your vitamins and minerals from a healthy varied diet. If you are not tolerating insoluble fibre during a flare up and have therefore reduced your intake of fruit and vegetables you may want to take a general multivitamin supplement until you return to your usual diet. During a flare up of UC you may have a poor food intake. If this continues for more than a week and you are losing weight your doctor or dietitian may recommend a supplement drink to prevent further weight loss.
Further information
Crohn’s and Colitis UK (NACC)
1 Bishop’s Square, Hatfield,
AL10 9NE
0300 222 5700
Website: www.crohnsandcolitis.org.uk
Foods to add and avoid during a flare up – Quick reference guide
| Food to add | Food to avoid | |
| Meat | Turkey, beef, lamb, game meats (opt for low fat cuts | Pork, duck, goose, processed meats such as salami, sausages, and meat pies. Fried or spicy meats. |
| Fish | Poached, steamed, boiled or roasted | Fried fish, especially in breadcrumbs or batter. Fish that has been smoked, pickled or marinated in fat and/or spices. |
| Eggs | Omelettes, poached, boiled or scrambled eggs. Egg mayonnaise. | Fried eggs, scotch eggs |
| Dairy *only avoid if avoiding lactose | Lactose free milk or suitable alternative e.g. soya, rice or almond milk Lactose free yoghurts or suitable alternatives e.g. soya yoghurts Hard cheeses such as cheddar, Edam. | Cow’s milk* Yoghurts and Ice-cream made with cow’s milk* Soft cheeses* |
| Bread, pasta, rice and other grain products | White bread, white rice, white pasta, semolina, buckwheat, sago | Wholemeal, granary, barley or dark rye bread. Bread containing nuts and seeds Wholemeal pasta. Brown rice. |
| Vegetables | Root vegetables – potatoes, sweet potatoes, parsnips, swedes and carrots Aubergines, courgettes, pumpkins. | Peas, sweetcorn, beans and lentils, cabbage, brussels sprouts, cauliflower and broccoli Salad leaves and vegetables, raw onions, garlic and peppers. |
| Fruits | Peeled or cooked apples, pears, bananas, peaches and nectarines. Papaya, melon, avocado and mango. Fruit jellies. | Grapes, plums, oranges, grapefruits, cherries, tomatoes. Dried fruits, rhubarb |
| Breakfast cereals | Cornflakes, puffed rice cereals, porridge. | Wholegrain cereals, mueslis. |
| Drinks | Decaffeinated teas/coffees, inc. peppermint and fruit teas, fruit squash/juices (no bits) | Fizzy drinks, drinks containing sweeteners, Alcohol. Fruit juice with bits. |
