Cut and Push Removal of A Freka Percutaneous Endoscopic Gastrostomy (PEG)
Please note, this page is printable by selecting the normal print options on your computer.
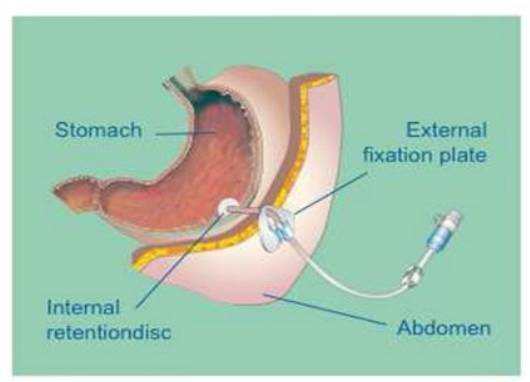
You have been asked to attend the Endoscopy Department at Milton Keynes Hospital to have your PEG tube removed or exchanged.
Why do I need my PEG to be removed or changed?
• It could be that you no longer require the PEG because you are managing to eat and drink orally.
• Your PEG tube has become worn or damaged.
It is not uncommon for PEG tubes to need changing. Some PEG tubes last for 1-2 years whilst others remain in place for significantly longer. The procedure only takes a few minutes and so you should only be in the endoscopy department for a short time.
What is the ‘Cut and Push’ method?
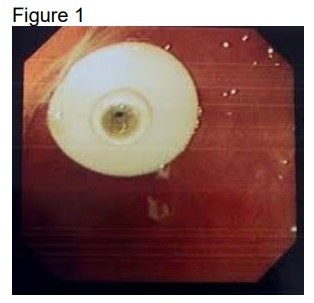
‘Cut and push’ describes a technique used to remove PEG tubes. The PEG tube is cut close to the skin and the circular piece of plastic (Internal disc on the inside of the stomach) is pushed into your stomach. It is approximately the size of a 10 pence piece. See figure 1.
What happens to the internal disc after it has been pushed into the stomach?
The internal disc will pass through your intestines and be passed out of your body when you open your bowels. You may not notice that the internal disc has been passed.
Are there any risks with the ‘cut and push’ method of removal?
There is a very small risk that the internal disc could get stuck in the bowel. This could then cause an obstruction and would require urgent medical attention. For this reason, before the procedure,
the doctor will ask you the following questions:
• Have you previously had any abdominal/ bowel surgery?
• Do you have Inflammatory bowel disease (Crohns disease or ulcerative colitis)?
• Do you regularly suffer from constipation?
If you answer yes to any of the above, your doctor may decide that the ‘cut and push’ method of removal is not suitable for you. The PEG can then be removed endoscopically.
What do I need to do in preparation for the procedure?
• Ensure that you have not eaten or had any feed via your PEG for 6 hours prior to the procedure.
• Ensure that you have not had any fluid orally or via your PEG for 4 hours prior to the procedure.
• Check that your PEG is advancing and rotating 360 degrees and if it is not, inform the doctor before the procedure.
• Bring slippers and a dressing gown with you.
What happens on the day of your appointment in Endoscopy?
• Before your PEG is removed the doctor will explain the procedure, including any associated risks. If you have any questions the doctor will be able to answer them.
• You will be asked to lay flat whilst the PEG is removed. This normally only takes a few minutes.
• Sedation is not required as the procedure is not normally painful.
• A dressing will be placed over the site as some patients may experience a small amount of leakage from the hole. The hole will normally close over after 48hrs.
• Your GP and community dietitian will be advised via letter that your PEG tube has been removed or exchanged.
Can I eat and drink after the procedure?
It is recommended that you wait 2 hours after the procedure before you eat and drink. After this time, you can eat and drink normally.
Will I be able to bathe straight away?
You can shower straight away; however, we would advise that you wait for 48hrs before taking a bath or swimming.
What if I am having my tube exchanged?
• A replacement tube will be inserted into the hole immediately after the PEG tube has been removed. The tube will be slightly different to your PEG tube, but this will be discussed with you after the change and the community nutrition nurse will be available to support you.
• You will be able to start feeding as normal 2 hours after the procedure.
• This type of feeding tube is changed at home by a community nurse every 3 months.
When to contact your GP?
• If the PEG site continues to leak after 7 days and the dressing needs to be changed frequently.
• If you have a temperature as this may indicate an infection.
IMPORTANCE NOTICE
If you have any of the following symptoms go to your local Accident and Emergency Department:
• Your abdomen is bloated, tender and painful
• You are vomiting
• You have constipation
It is possible that the internal disc has got stuck and may be causing an obstruction. You will need an urgent X-ray of your abdomen.
Please take this leaflet with you to the Accident and Emergency department.
Useful phone numbers:
Endoscopy: 01908 996460
Community Nutrition nurse: 0782 483335
Community Dietitians: 01908 995416
Nutrition Nurse: 01908 660033 bleep 1722
