Colonoscopy – The procedure explained
Please note, this page is printable by selecting the normal print options on your computer.
Introduction
You have been advised by your GP or hospital doctor to have an investigation known as a colonoscopy.
This procedure requires your formal consent. This booklet has been written to enable you to make an informed decision in relation to agreeing to the investigation. You will be required to sign a consent form on the day of the procedure, which is a legal document, therefore please read this booklet carefully beforehand.
If you are unable to keep your appointment, please notify the endoscopy unit as soon as possible. This will enable staff to give your appointment to someone else and to re-arrange another date and time for you.
You need to understand all the information, including the possibility of complications. There will be the opportunity to speak to a health care professional about anything that you do not understand on the day of the procedure before you sign the consent form.
What is a Colonoscopy?
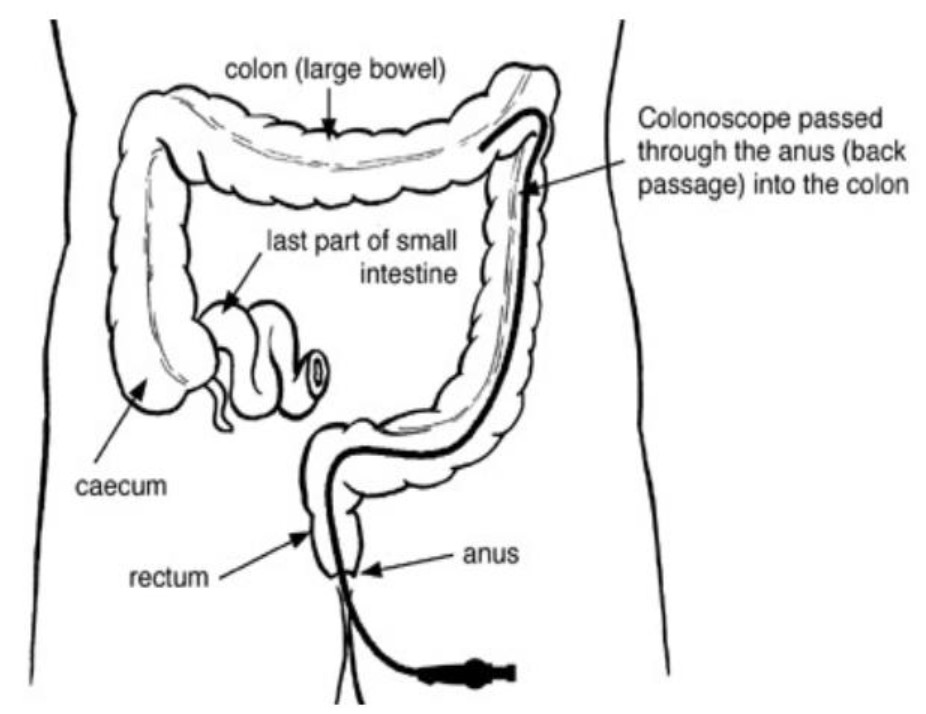
This is an examination of your large bowel (colon). It will be performed by an endoscopist; this may be a doctor or a specialist nurse who has been trained to do this procedure.
You will usually be offered sedation and pain relief to make the procedure as comfortable as possible for you.
This procedure is a very accurate way of looking at the lining of your large bowel (colon), to see if there is any abnormality. This test also allows us to take samples (biopsies) if necessary; this is painless. The samples will be looked at under the microscope to help diagnosis and these will be retained by the pathology unit. Photographs may be taken and retained in your case notes.
The instrument used for this procedure is called a colonoscope which is a long flexible tube with a small camera and light at the end that relays pictures back to a television screen. This enables the endoscopist, to have a clear view and to check whether or not disease or inflammation is present.
What is a polyp?
A polyp is an overgrowth of cells that make up the lining of the bowel. Some polyps have a stalk and look like a cauliflower floret, whereas others are flat without a stalk. Polyps when found are generally removed or sampled by the endoscopist as they may grow and later cause problems. Flat polyps are sometimes a little more difficult to remove.
Polypectomy
A polyp may be removed in one of three ways using an electrical current known as diathermy to burn the polyp free of the bowel wall.
For polyps with a stalk, a snare (wire loop) is placed around the polyp and diathermy is applied to burn the polyp from the lining of the bowel wall. It is then removed and sent to the pathology unit to be looked at under the microscope.
Flat polyps (without a stalk) can be removed by a procedure called Endoscopic Mucosal Resection or EMR. This involves injecting the lining of the bowel with special solution in the area that surrounds the flat polyp. This raises the polyp to allow a snare to pass around it and diathermy is applied to burn the polyp from the lining of the bowel wall.
For smaller polyps a biopsy forceps is used. These have two cups which capture the polyp and then diathermy is applied, again burning the polyp from the bowel wall.
Why do I need to have a colonoscopy?
- You may have been advised to have this procedure to try to find the cause of your symptoms, help with treatment, and if necessary, to decide on further investigations.
- Follow-up inspection of previous disease.
- Assessing the clinical importance of an abnormality seen on an x-ray or scan.
Are there any alternatives to a colonoscopy?
A colonoscopy is recommended as it is the best way of diagnosing most problems with the large bowel.
Another option is a bowel scan called CT Pneumocolon or CT colonography. However, if your doctor finds a problem, you may still need a colonoscopy to treat the problem or perform biopsies.
How do I prepare?
To get a clear view of the colon it is important that the bowel is empty of faeces. You will be sent information on how to do this with your appointment. You will be given detailed instructions about stopping certain medication such as iron tablets and constipating agents and as to what you can and can’t eat during the days before the procedure and then you will be given a laxative solution to clear your bowels. It is important that you follow the instructions leaflet sent to you with the laxative.
What about my medication?
Routine medication
If you are on any medication, especially blood pressure tablets, you should take these with a small amount of water as usual.
If you are taking iron tablets, you must stop taking them one week prior to your appointment. If you are taking a stool bulking agent such as Fybogel, Regulan, Proctofibe, or constipating agent such as Loperamide (Imodium), Lomotil or Codeine Phosphate you must stop taking them 4 days before your appointment.
Diabetes
If you have diabetes and control this with insulin or tablets, please ensure that the Endoscopy Unit is aware so that your procedure can be booked for the beginning of the list.
Please see guidelines in the bowel preparation leaflet that we send you with the bowel preparation.
Anticoagulants / Antiplatelets
If you are taking blood- thinning medicines, such as Warfarin, Dabigatran, Heparin, Deltaparin, Apixaban, Clopidogrel, the dose of these may need to be altered or stopped before your procedure. You may also need to have blood tests before your procedure. If the referring doctor did not give you instructions, you may be referred to the bridging clinic for advice on stopping your medication. If this is required, this will be arranged for you by the referring clinician or the endoscopy booking coordinator.
Contraception
If you are taking the oral contraceptive pill, you should take the pill at least three hours before taking the bowel cleansing preparation, and then continue taking the pill as normal from the next day. Alternative contraceptive precautions should be taken for the rest of your cycle.
If you have further questions or concerns, please contact your GP or practice nurse for clarification.
Epilepsy
If you suffer with Epilepsy, please contact your neurologist to discuss the procedure and decide on an individual plan for your epilepsy medication during the bowel preparation.
If they advise you to continue your oral antiepileptic medication, please take them 2 hours before or after taking your bowel prep (Moviprep, Kleanprep or Picolax).
What to bring with you?
Along with your appointment letter you will have received a health questionnaire. Please complete it and bring it with you.
We have enclosed a copy of your consent form for you to read. Please do not sign this until the day but read it carefully beforehand. The endoscopist or nurse will discuss the procedure, what is going to happen, any risks and any serious or common side effects. You will be given the opportunity to ask any questions before you sign the consent form. This will be done before you are taken to the procedure room.
You will also need to bring a dressing gown and a pair of slippers.
How long will I be in the Endoscopy unit?
You should expect to be in the unit for approximately 3-4 hours. Please note that the time of your appointment is not the time that the procedure will be performed.
How long you will be in the unit will depend on how quickly you recover from the procedure, the sedation you may have had and on how busy the unit is.
The unit also looks after emergencies and these can sometimes take priority over outpatient procedures.
You should be kept informed of any delays, but if you have any questions or concerns, please ask a member of the staff.
What happens when I arrive?
After checking in at reception, a qualified nurse will welcome you and take you to the admissions area where you will have a brief medical assessment.
Please note that the endoscopy unit operates a same sex environment and your relative may not be able to accompany you past the waiting area unless there are exceptional circumstances.
In the admission room, you will be asked some questions regarding your medical and surgical history to confirm that you are fit to undergo the procedure and about your arrangements for getting home. The nurse will make sure that you understand the procedure and discuss any questions you may have.
Your blood pressure, heart rate, respiration and oxygen levels will be recorded. If you have diabetes, your blood sugar level will also be checked and recorded.
If you have chosen to have sedation, which will be given later, the nurse will insert a cannula (a small plastic tube) into a vein in your hand or arm.
Before the procedure you will be asked to put on a hospital gown. Dignity shorts are available if you would like to wear them.
All your belongings will be kept with you throughout your procedure to prevent anything being lost. It is advisable to leave any valuables at home as we do not accept responsibility for them.
Intravenous sedation
You can chose to have a sedative (usually Midazolam) and a painkiller (usually Pethidine or Fentanyl) and sometimes something to relax your bowel (usually Buscopan) which will be administered via the cannula into your vein, and will make you lightly drowsy and relaxed, but not unconscious. This means that you will still hear what is said to you and therefore, will be able to carry out simple instructions during the procedure. Some people do not remember anything about the procedure once the effects have worn off.
Whilst you are sedated, we will monitor your breathing, respiration, and pulse rate via a finger probe, so that any changes can be recorded and dealt with accordingly. You will also be given some oxygen via a nasal sponge into your nostril. Your blood pressure may also be checked and recorded.
If you are having sedation, you must arrange for a responsible friend or relative to collect you and stay with you overnight. You should not drive, return to work, operate machinery, or drink alcohol for 24 hours after the procedure, nor should you make any important decisions. The reason for this is that the sedation may, despite the fact that you may feel perfectly normal, still be in the body and may impair your judgement.
Alternatively, you can choose to have Entonox (gas and air) which provide pain relief when inhaled. You will be able to drive half an hour after your procedure and will not need an escort.
The colonoscopy procedure
After signing your consent form in the admission area, you will be escorted to the procedure room, you will be introduced to the team and a verbal safety checklist (called “WHO”) will be done.
You will be asked to lie on your left side with your knees drawn up towards your chest. If you wish, you will be able to watch the procedure on the television screen. If you wear spectacles you may be asked to remove them. The finger probe will be placed on your finger and the sedation will be given through the cannula in your hand. The nasal sponge will be positioned in your nose.
The endoscopist will perform a finger examination of your back passage before inserting the scope. The colonoscopy involves moving the scope around the entire length of your large bowel. Air is gently passed into the bowel to assist the passage of the colonoscope. There are some naturally occurring bends in the bowel and negotiating these, may be uncomfortable for short periods of time. However, the sedation should minimise any discomfort. Entonox should also be offered to relieve the discomfort.
During the procedure it is sometimes necessary to ask you to turn onto your back, onto your right side and sometimes onto your tummy. A nurse may also press at various times on your tummy. This is done to help the endoscopist move the scope on and to make you more comfortable. During the procedure, biopsies or polyps may be taken from the colon and sent to the pathology unit. The examination usually takes between 30 and 60 minutes.
Milton Keynes University Hospital is a teaching hospital and there may be a student and/or a trainee in the room or a supervised trainee may be doing your procedure. If you have any concerns or objections, please contact the Endoscopy Unit prior to your test.
Aftercare
You will be resting on a bed in the recovery area until you have woken up sufficiently to have a drink. You will have your blood pressure, pulse, respiration, and oxygen levels checked until you have recovered from the initial effects of the sedation (which normally takes 30-60 minutes). If you have diabetes, your blood sugar level will be checked.
You will be encouraged to get rid of any wind that you have so that you will be more comfortable. You will then be asked to get dressed and move into the seated area where you will be offered a hot drink and biscuits.
When will I know the results?
Before you leave the unit, a nurse or the endoscopist will discuss the findings, any medication, further investigations, and follow-up arrangements that you may need. Due to the sedation temporarily affecting your memory, you may wish to have your responsible adult with you when you are given this information.
If a sample (biopsy) has been taken during the procedure, the results may take several weeks. Details of results and any necessary treatment should be discussed with your general practitioner (GP) or the consultant who referred you to have the test.
Before leaving the unit, you should receive a copy of your consent form, written information on aftercare and follow up.
Being collected after the procedure
If you are having sedation, the person collecting you must come to the unit to collect you. We advise that they park in the multi-storey car park before reporting to the Unit.
Are there any risks?
Colonoscopy is considered to be an invasive procedure and because of this there are some risks associated with it. These occur infrequently, but we wish to draw your attention to them in order to help you make your decision.
The doctor or specialist nurse who has requested the test will have considered this already. The risks must be compared with the benefit of having the procedure carried out.
The possible complications of colonoscopy are listed below. Any numbers which relate to risk are from studies of patients who have had this procedure. Your doctor will tell you if the risk of complications is higher or lower for you.
- Allergic reaction to the equipment, materials, or sedatives. The endoscopy team is trained to detect and treat any reactions that might happen. Let the admitting nurse or the endoscopist know if you have any allergies or if you have reacted to any drugs or tests in the past.
- Breathing difficulties or heart irregularities, as a result of reaction to sedation or inhaling secretions such as saliva. To help prevent this from happening, your respiration and oxygen levels will be monitored, and a suction device will be used to clear any secretions. Rarely, a heart attack or stroke (loss of brain function resulting from an interruption of the blood supply to the brain) can happen if you have serious medical problems.
- Perforation – making a hole in the colon (risk: less than 1 in 1,000). The risk is higher if a polyp is removed (risk: less than 1 in 500) and for dilatation stricture and stent placement (2-5 in 100). This is a serious complication. You may need surgery which can involve forming a stoma (bowel opening onto the skin).
- Bleeding from a biopsy site or from minor damage caused by the endoscope (risk: less than 1 in 1,000). This usually stops on its own.
- Bleeding, if a polyp is removed (risk: 1 in 100). Bleeding usually stops soon after a polyp is removed. Sometimes the bleeding can happen up to two weeks after the procedure. If you are taking blood- thinning medicines, such as Warfarin, Dabigatran, Heparin, Dalteparin, Apixaban or Clopidogrel and have a polyp, the endoscopist will not usually remove it unless your medication has been adjusted in advance and your INR (International Normalised Ratio) levels are safe.
- Incomplete procedure. This can happen due to a technical difficulty, food or blockage in the lower digestive system, complications during the procedure, or discomfort. Your doctor may recommend another endoscopy, or a bowel scan called CT Pneumocolon or CT Colonography.
- Sedation can occasionally cause problems with breathing, heart rate and blood pressure. If these problems do occur, they are usually short lived. Careful monitoring by the endoscopy team ensures that any potential problems can be identified and treated quickly. Older patients and those with significant health problems, such as breathing difficulties due to a bad chest, may be assessed by a doctor or specialist nurse before having the procedure.
You should discuss these possible complications with your doctor if there is anything you do not understand.
What to do if you feel unwell once at home:
If you experience pain that is severe and persistent, or you are passing significant amount of blood or clots; you must then seek urgent advice from the Endoscopy Department between 09:00 and 17:30 (01908 996460).
Outside these hours, please call a nurse on Ward 8 (01908 996395) for advice or go to your nearest A&E department.
References for the information contained within this leaflet can be obtained if required from the author.
People are unique and the alternatives, risks and benefits will of course vary from person to person. We hope this leaflet will support the information you have already received from your doctor in enabling you to make an informed decision about your care. If you have any further questions, please ask.
