Cardiac Angiography Unit Pacemaker Implant Pre-Procedure
Please note, this page is printable by selecting the normal print options on your computer.
Important points to remember Please read this information book carefully, if you have any questions, please bring these with you to your pre-assessment appointment.
- You should take all your normal medications as prescribed except anticoagulation (“blood thinners”) such as Warfarin, Apixaban, Dabigatran, Rivaroxaban and Edoxaban.
- Instructions for anticoagulation medication advice should be given to you by the team. If you take Warfarin, Apixaban, Edoxaban, Dabigatran or Rivaroxaban and unsure of the exact advice please phone the angio department on 01908 996539 and ask to speak to one of the nurses for advice, at least one week before your procedure.
- You may wish to postpone taking any ‘water tablets’ (diuretics) on the day of the procedure and take them after your procedure has been performed.
- Please bring all the medications you are taking to the hospital with you.
- If you are a diabetic, please inform the nursing staff who can monitor your blood sugar levels whilst you are not eating and drinking
- Please do not eat or drink anything on the day of your appointment unless the nurse or doctor tells you it is safe to do so. This allows for the safe use of conscious sedation during your procedure. However, you may drink sips of water up to your procedure time.
- Your admission letter will give you details of where you will be admitted on the day of your pacemaker insertion.
The morning of the test We ask that your relatives/friends drop you off at Cardiology reception at the time of your appointment.
Relatives / friends are not permitted into the day ward, but they will be contacted when the nurses are happy that you are fully recovered and ready to leave .
On arrival, please report to the Cardiology department at the rear of the hospital site where you will be able to park in the Cardiology patient ‘pay and display’ car park. It is important that you arrive on time in the morning.
You will be taken to the Day Ward in the Cardiac suite. On arrival to the day ward, you will be asked to change into a gown ready for your procedure. Bring a dressing gown and comfortable footwear.
We advise that you leave all valuables at home. The nurse will check all your details and discuss the procedure with you.
Antibiotics will be given to you before the procedure through a cannula in your arm and if the doctor feels it necessary maybe on discharge home.
Every effort is made to ensure your waiting time is kept to a minimum. Occasionally delays can occur; the nursing team will keep you informed of any changes.
The heart:
The normal adult heart has a regular heartbeat which is within 50 and 100 beats a minute.
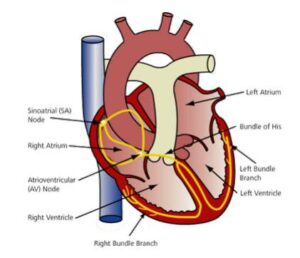
The heart has four chambers as shown below.
The heart has a natural pacemaker (sino-atrial node) this group of cells is on the right side of the heart and transmits electrical impulses across the two small chambers of the heart (atria).
Another group of cells called the atrio-ventricular node (AV node) are positioned above the two large chambers of the heart (ventricles).
As the electrical impulses pass from the AV node to the ventricles this causes them to contract – this is your heart beat.
What is a pacemaker?
A pacemaker is a small, battery powered device that is implanted permanently into the body. The pacemaker monitors the electrical impulses in the heart and, when needed, delivers electrical stimuli to make the heartbeat (contract) in a normal rhythm.
When is it used?
A pacemaker is used when the heart beats too slowly (bradycardia) or has other abnormal rhythms (arrhythmias). In some cases, pacemakers are also used to treat symptoms of breathlessness from heart failure.
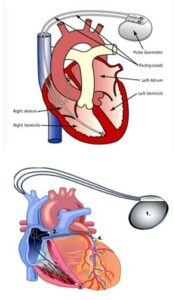
- Pulse generator 2. Right Atrial wire 3. Right ventricle wire 4. Coronary sinus pacer wire.
Pacemakers are designed to meet the specific needs of each individual patient.
- Rate responsive pacemakers These pacemakers may be programmed to increase or decrease your heart rate to match your activities (walking, running, resting)
- Single chambered pacemakers These pacemakers use only one lead positioned into the right upper chamber (right atrium) or the right lower chamber (right ventricle).
- Dual chambered pacemakers These pacemakers have two leads. One positioned in the right atrium and the other one in the right ventricle.
- Non-standard dual chambered pacemakers These pacemakers have leads that may be placed in multiple positions in the right ventricle. Your cardiologist is likely to have discussed reasons for this in advance. This procedure often takes more than 1 hour.
- Cardiac Resynchronization Therapy Device (CRT). These pacemakers can have 2 to the 3 leads depending on your underlying heart rhythm, a lead placed in the right atrium, one in the right ventricle and another one through the coronary sinus (from the right atrium) lead is deployed into a suitable vein.
If you already have a pacemaker, you may be having your box (pulse generator) changed in order to replace the battery. This is a shorter procedure than your initial pacemaker, and you will have been informed by cardiac physiologist that they are referring you for this.
The procedure:
The procedure is carried out in a specially designed room which is set up like an operating theatre.
There will be a number of staff present throughout the procedure including a Cardiologist, Nurses, Cardiac Physiologists and Radiographers.
There may be staff present undergoing training.
You will be asked to walk from the Day Ward area into the Lab area; if you are unable to walk we will provide a wheelchair or trolley.
The procedure normally takes about 1 hour to 1 and a half hours to perform, depending on which type of pacemaker you are having fitted or if the procedure is for a box change.
You will be awake throughout the procedure, but medication can be given to help you relax.
Once inside the room you will be asked to lie on the operating table.
An x-ray machine may take pictures during the procedure.
A local anaesthetic will be injected into the area where the doctor will make a small incision for the pacemaker.
The pacing leads are entered into the heart this will be x-rayed during placement to ensure good positioning.
At this point, the doctor tests the lead to see if this location is suitable.
You will hear the team calling out numbers whilst testing the lead, this refers to the lowest amount of energy needed to stimulate your heart to beat, helping your doctor find the best position for the lead.
This is called the threshold. Once the leads are in position further X-rays will be taken, you may be asked to take deep breaths and cough while your doctor observes an X-ray of your heart.
This is all to ensure proper and secure placement of the leads. Once the leads are in position your doctor will plug these into the pacemaker and slip the pacemaker into the small pocket made beneath the skin of your upper chest.
The pocket is closed with stitches to complete the procedure.
You will be monitored closely during the procedure, if you are having any discomfort, please inform your nurse or doctor. You will then be taken back to the day ward.
After the procedure:
When you return to the day ward your blood pressure and pulse will be checked by a nurse.
A dressing may be applied over the pacemaker site and the nursing staff will observe this. Please inform the nursing staff if you are in any significant pain after the procedure. As the local anaesthetic effect begins to fade, a dull ache is normal for a few days after a pacemaker implantation.
You will be offered something to eat and drink as soon as the nurse feels that you are ok.
You will need a pacemaker check before you go home to see if the pacemaker function is correctly set for your needs, and a further x-ray will be performed to document the final position of the lead/s and exclude any complications prior to discharge.
You will need a relative or friend who is able to collect at any time on the day of the procedure and someone to stay at home with you over night.
Future appointments:
Once you have a pacemaker you will be asked to return to the department at frequent intervals to assess the pacemaker’s battery life and make any changes to the devices parameters that might be needed.
As the battery life on the device decreases these visits could increase in frequency until you are asked to come back and have a new pacemaker battery fitted.
Pacemaker batteries last anything from 8-12 years depending on the indication but not everyone’s pacemaker is used all the time.
Are there any risks? There are some risks associated with having a pacemaker inserted. These may include:
- Bleeding
- Infection
- Pneumothorax – this is when air gets into the lining of the lungs. If this occurs you may experience some shortness of breath and discomfort and could be admitted to hospital to treat this. Often this is managed with oxygen supplementation and resolves without intervention.
For some patients, having to lie still on the procedure table for the length of the procedure may cause some discomfort or pain.
There may be other risks depending on your medical condition. Please discuss any concerns with the doctors or nursing staff before the procedure.
You will be given more advice on the risks when you are discharged, however, if you experience any of these you may need urgent medical attention.
For any other information or if you have any questions with regards to your procedure, please contact the nurses on the cardiac angiography unit on the number below.
Contact details:
Milton Keynes Hospital NHS Foundation Trust Cardiac Angiography Unit Department of Cardiology Milton Keynes Hospital Standing Way Milton Keynes MK6 5LD
Cardiac Angiography Unit 01908 996539 (Monday to Friday 8am-4pm)
Coronary Care Unit/ Ward 17 01908 996419 (24hrs 7 days)
Cardiology Department Reception 01908 997197 (Monday to Friday 9am-5pm)
Cardiac Physiologists. 01908 997200 (Monday to Friday 08:30am –16:30pm please leave a voicemail).
