Bronchoscopy & EBUS
Please note, this page is printable by selecting the normal print options on your computer.
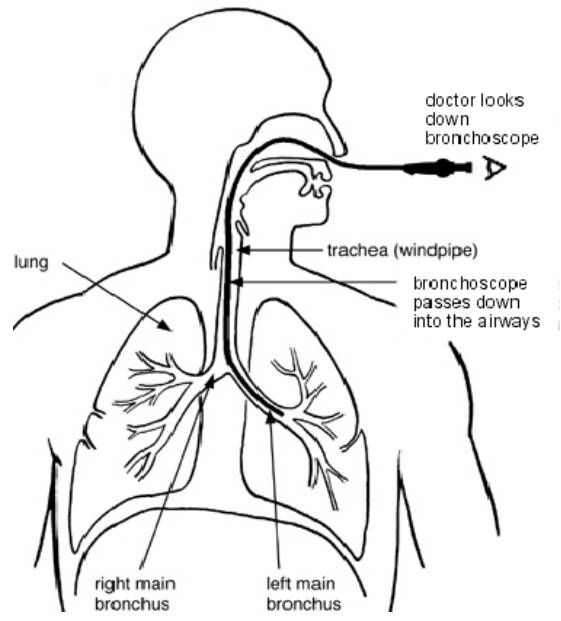
Diagram of a Bronchoscopy Procedure
You have been advised to have an investigation known as a Bronchoscopy (examination of the lung). This procedure requires your formal consent. This leaflet has been written to enable you to make an informed decision in relation to agreeing to the investigation. You will be required to sign a consent form on the day of the procedure, which is a legal document, therefore please read this leaflet carefully.
You need to understand all the information, including the possibility of complications.
There will be the opportunity to speak to a healthcare professional about anything that you do not understand on the day of the procedure before you sign the consent form. If you are unable to keep your appointment, please notify the Endoscopy Admission Office on 01908 996 939 as soon as possible. This will enable staff to give your appointment to someone else and re-arrange another date and time for you.
What is a Fibreoptic Bronchoscopy?
A Fibreoptic Bronchoscopy is a procedure (using a camera) done under local anaesthesia and sedation, for examination of breathing tubes (airways) and if indicated, to take samples. To do this, the doctor uses a ‘bronchoscope’, which is a long flexible tube, about the width of a thin pencil, with a bright light at the end.
During a Bronchoscopy, a bronchoscope is passed through your nose or mouth, past your larynx (voice box), down your trachea (windpipe) and into the bronchi. The doctor can look at the images taken by the bronchoscope to check whether any disease is present in your lungs.
What is an Endobronchial Ultrasound Scan Biopsy (EBUS)?
An endobronchial ultrasound (EBUS) procedure is like a bronchoscopy. An EBUS scope has an ultrasound at its tip and allows the doctors to look outside the breathing tubes. An ultrasound uses soundwaves to produce a picture. This helps in taking biopsy samples from the lymph nodes and the areas outside the breathing tubes.
Why do I need to have a Bronchoscopy?
Having a Bronchoscopy means that your doctor will be able to get exact information about your condition which will help plan the best treatment for you.
Are there any alternatives to a Bronchoscopy?
Having a Bronchoscopy is the safest and quickest way to look at the bronchi and take biopsies. It is the only procedure that allows us to easily collect salt-water samples (BAL) from the lung. An alternative to this procedure is an operation under general anaesthetic where a biopsy of the lung or mediastinal lymph glands is carried out. This is sometimes necessary if the bronchoscopy fails to provide the answer. The risks of general anaesthesia are higher, and the procedure may take longer than the Bronchoscopy.
Another option is for the needle to be inserted through the chest wall under local anaesthetic to take a biopsy. This is only possible if the area to be biopsied lies close to the chest wall. The procedure carries a higher risk of the lung collapsing and bleeding rather than a Bronchoscopy. You may also want to discuss the effects of not having the procedure with your doctor.
How do I prepare?
Please do not eat or drink anything for six hours before your procedure. If you are a smoker, please do not smoke on the day of the procedure.
What about my medication?
- Routine Medication: If you are on any medication, especially blood pressure tablets, you should take these with a small amount of water as usual.
- Anticoagulants / Antiplatelets: If you are taking Warfarin, or any blood-thinning medicines, such as Apixaban, Rivaroxaban, Dabigatran, Ticagrelor and Clopidogrel, need to be stopped before your procedure. Your consultant should have informed you. You may also need to have blood tests before your procedure. If the referring doctor did not give you any instructions, please contact the Consultant’s Secretary through switchboard (01908 660033).
- Diabetes: If you have diabetes and control this with insulin or tablets, please ensure that the Endoscopy Unit is aware so that your procedure can be booked for the beginning of the list. You will need to omit your diabetes medication during your “Nil by Mouth” phase. Your usual medication can be recommenced after the procedure once you are eating again. You may want to bring a sandwich with you to eat after the procedure with your usual diabetes medication. If you have any further concerns, please contact your Diabetic Specialist Nurse well in advance of the procedure for advice.
What to bring with you?
Along with your appointment letter you will have received a health questionnaire. Please complete it and bring it with you. Please wear loose fitting, easily washable clothing and leave your valuables at home.
How long will I be in the Endoscopy Unit?
Please note that the time of your appointment is not the time that the procedure will be performed. You may be waiting some time before your procedure is carried out. Some procedures take longer than expected and emergencies take priority.
The length of time you will be in the department depends on how quickly you recover from the procedure, the sedation you may have had and on how busy the unit is.
What happens when I arrive?
After checking in at reception, a qualified nurse will welcome you and take you to the admissions area where you will have a brief medical assessment. Please note that the Endoscopy Unit operates a same sex environment and your relative may not be able to accompany you past the waiting area unless there are exceptional circumstances.
In the admission room, you will be asked some questions regarding your medical and surgical history to confirm that you are fit to undergo the procedure and about your arrangements for getting home. The nurse will make sure that you understand the procedure and discuss any questions you may have. Your blood pressure, heart rate, respiration and oxygen levels will be recorded. If you have diabetes, your blood sugar level will also be checked and recorded.
The Consultant or the Registrar will come and explain to you the procedure and take your written consent (if not already taken in clinic). You can ask any questions you have regarding the procedure. If you wear glasses or dentures, you will be asked to remove them when you enter the procedure room. All your belongings will be kept with you during your procedure to prevent anything being lost. You are advised to leave your valuables at home as we do not accept responsibility for them.
This procedure usually involves the use of sedation, which will make you feel relaxed and sleepy during the Bronchoscopy. A sedative called Midazolam will be administered through an IV cannula (a plastic tube which is placed in a vein in your arm/hand).
It is important that a responsible adult accompanies you home and stays with you overnight. If you have not been able to make these arrangements, you will not be able to have the procedure.
You should not drive, return to work, operate machinery, or drink alcohol for 24 hours after the procedure, nor should you make any important decisions. The reason for this is that the sedation may, even though you may feel perfectly normal, still be in the body and may impair your judgement.
During the Bronchoscopy procedure
A nurse will stay with you and will monitor you throughout the procedure. In the Bronchoscopy room you will be made comfortable on a hospital bed in a sitting or lying down position. The doctor may give you an injection of a sedative into a vein in your arm to make you feel sleepy and relaxed.
A local anaesthetic will be sprayed in your mouth towards the back of your throat. This numbs your throat, and it may feel like you cannot swallow. For longer procedures sometimes an injection of local anaesthetic is given in the throat area (below the Adam’s apple). This permits the main central windpipe to be numbed and may provoke a bitter taste at the back of the throat which will anaesthetise this area as well. The discomfort lasts for about 10 – 15 seconds. This achieves the same outcome of numbness of the throat.
If the Bis to be performed through the nose, local anaesthetic jelly will be inserted into your nostrils; this makes it more comfortable to have the bronchoscope tube in your nose.
As the bronchoscope is passed through your nose or mouth and down the back of the throat, more local anaesthetic will be sprayed onto the larynx (voice box). This may make you cough a little. However, as the local anaesthetic takes effect, your throat will relax, and the coughing should ease. When the bronchoscope enters the lungs, there is no need to worry; there is plenty of room to breathe around it as the tube is very thin.
During the procedure you will be given extra oxygen through a soft plastic tube placed just inside your nostril. A plastic ‘peg’ will be placed on your finger to monitor your heart rate and oxygen levels throughout the procedure. The Bronchoscopy usually takes 20-30 minutes to complete.
Other investigations that may be carried out
During the Bronchoscopy it may be necessary to have a ‘wash’, broncho-alveolar lavage (BAL), or a biopsy. These are explained below:
‘Wash’ or broncho-alveolar lavage (BAL): Performing a wash involves passing a small amount of salty water through the bronchoscope into a certain part of the lung and sucking it back out again. The fluid that is sucked back out is sent for laboratory examination. The broncho-alveolar lavage (BAL) is a similar procedure but uses a larger amount of fluid (up to 180mls).
Biopsy: This involves passing a wire down the bronchoscope with a small pincer at the end. The pincer is used to take a tiny piece of lung (biopsy), which is then sent for laboratory examination under a microscope. There are four different types of biopsies: endobronchial (EBB), transbronchial (TBB), transbronchial needle aspiration (TBNA) and Endobronchial ultrasound guided transbronchial fine needle aspiration (EBUS-TBNA).
You should not feel any pain with these biopsies:
- Endobronchial (EBB) – During this biopsy, a small piece of tissue is gently pinched off the surface of the lining of the bronchi. There are few side effects with this biopsy.
- Transbronchial (TBB) – This biopsy is taken from deeper into the lung and carries a higher risk than an EBB (please see ‘Potential risks and complications of the procedure’). This type of biopsy still involves gently pinching a small piece of tissue, which is taken from the lung.
- Endobronchial Ultrasound Guided Transbronchial Fine Needle Aspiration (EBUS-TBNA) – This procedure uses a special bronchoscope with ultrasound scanning built into it. This allows the area beyond the air passages to be evaluated and samples from lymph glands obtained under ultrasound control.
Some people may need a lymph gland biopsy, which is known as ‘transbronchial needle aspiration’. The lymph glands sit outside the lungs in the central part of the chest; however, they cannot be reached directly with a bronchoscope. Instead, small samples of tissue can be taken from the lymph glands by passing a fine needle through the trachea or bronchi.
The risks are like the other types of biopsies mentioned above but are less common. One additional risk is that of ‘mediastinitis’, which is inflammation, and possibly infection, of the central part of the chest (the ‘mediastinum’). If this develops you will experience some pain or discomfort in the centre of the chest and you will need to be admitted to hospital for treatment with intravenous antibiotics (given directly into a vein).
Aftercare
While you are in the recovery room, you may stay on the oxygen for anything between 15 minutes and one hour. A nurse will also record your blood pressure and your pulse rate. You will be kept in the recovery room for about two hours. After two hours, you will be offered a drink and discharged home with a responsible adult.
What do I do once I get home?
If you have had sedation, it is important that you do not do any of the following in the 24 hours after your test:
- Drive
- Operate machinery or domestic appliances, as your reaction times may be slowed down
- Drink alcohol, as this would increase the effect of your sedatives and make your reactions even slower
- Make any instant decisions
- Sign legal documents
- Do any energetic exercise or lift heavy weights.
Please follow any special instructions that your doctor or nurse might give you. When you get back from your test, you should stick to light meals and warm drinks for the rest of the day. Hot drinks will make your throat sore.
When do I know the result?
After the Bronchoscopy has been carried out the doctor may be able to tell you what he/she has seen. However, the full results of the test will not be available until your follow-up outpatient appointment (or during your hospital stay if you are an inpatient), as it can take up to seven days to process the results of biopsies and washes.
It is a good idea to have someone with you when you talk to the doctor after the procedure because the sedation can make you forget what is discussed. Your memory will return to normal when the sedation wears off fully, usually within 24 hours.
Is a Bronchoscopy safe?
A Bronchoscopy is a relatively safe procedure. The chance of having a complication is small. As medical procedures are all associated with a degree of risk, hospitals must tell patients about the potential risks and complications involved, even if the risks are small.
Common minor complications include:
- Sore throat and hoarse voice – this is due to the bronchoscope rubbing the lining of your throat and should disappear within 48 hours. Drinking plenty of fluids or sucking sweets may help relieve the symptoms.
- Nosebleed or soreness – this is due to the bronchoscope rubbing the lining of the nose and should disappear within 48 hours.
- Slightly blood-stained phlegm – this may occur if biopsies have been taken but should clear up within 24-48 hours. If it continues, please contact your hospital doctor.
- Fever, flu-like symptoms or aching across the lungs – these symptoms can occur and last for 24-48 hours. Usually, they will settle by taking paracetamol. If these symptoms continue for several days, please contact your hospital doctor as you may have developed a chest infection.
- A drop in your oxygen levels can occur during the procedure but does not usually have long lasting effects. Your levels are constantly monitored during and after the procedure, so that additional oxygen can be given if necessary.
Rare complications: Chest infection in less than one per cent (1%) of cases.
Potential complications associated with biopsies:
- Major bleeding can occur from the area where the biopsy was taken. This may need an overnight stay in hospital for observation, and in rare cases, a blood transfusion. Major bleeding can occur in one in every 500 people who have a biopsy. This is less than 1% of cases.
- If you have had a transbronchial biopsy (TBB), you will need a chest X-ray after the procedure. In 5-10 out of every 100 people who have this type of biopsy (5-10%), a complication known as a ‘pneumothorax’ can occur, and this is seen on the chest X-ray. This happens when air escapes from the lungs through a small hole created by the biopsy, instead of the air leaving through the nose as normal.
This air ends up trapped in the space between the lung and the chest wall because it cannot escape quickly. However, the small hole made by the biopsy usually heals within a few days and air stops leaking from the lung. The lung will gradually then expand back to its original size. If this is the case, an overnight stay in hospital for observation is usually all that is needed.
- In up to 25% of patients who develop a pneumothorax, the leak is large enough that the air needs to be removed. The air is either removed using a needle and syringe, which is inserted into the chest to remove the air, or by using a tube called a ‘chest drain’. If this is the case, you will need to remain in hospital until the lung repairs itself and the chest drain can be removed.
Please note that you will be given information about any additional procedures either in clinic (in ward if in-patient) or while taking consent.
What to do if you feel unwell?
Coughing up small streaks of bloods is normal after having a bronchoscopy. However, if you have chest pain or increased breathlessness after the procedure, please contact your GP. If you have these symptoms outside of hours, please go to your nearest A&E Department.
