Back and Pelvic Girdle Pain in Pregnancy Advice and Exercise
Please note, this page is printable by selecting the normal print options on your computer.
About 1 in 5 pregnant women are affected by pelvic girdle pain to some degree. It is common but not normal or to be expected during pregnancy. It is important to remember it may not get worse and with treatment and support early in pregnancy it can be managed well. It does not mean you cannot have a normal labour and delivery.
This leaflet is designed to provide you with advice and practical measures to assist you in reducing your pain and symptoms.
Causes of back pain and pelvic girdle pain in pregnancy
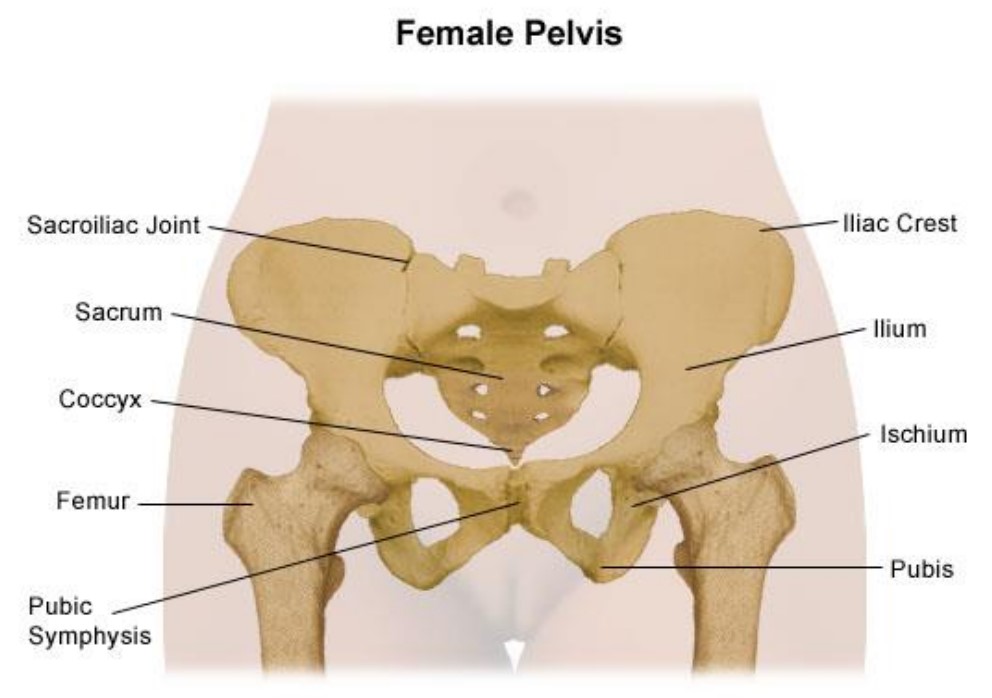
Pregnancy causes numerous changes in your body. These include changes in your posture and centre of gravity, increased weight, stretching of muscles around the tummy, and the ligaments around your joints softening and become more elastic.
These are a normal part of pregnancy and not usually the cause of pain. Sometimes the physical changes can contribute to pain, however, there are also other issues like how we are feeling – happy, sad, anxious, stressed, alongside our previous experiences which can increase our pain. It is important to address and be aware of all the factors that contribute to pain to help manage it better.
Common presenting signs and symptoms
The signs and symptoms can vary greatly between patients. Some people may find some activities aggravate pain such as:
- Walking (especially up or downhill and uneven ground)
- turning over in bed
- Negotiating stairs
- in/out of the car or bath
- Pain on sit to stand
Symptoms could feel like:
- Clicking or grinding in the joints
- Sensation of joints being ‘stuck’
- Sometimes restricted ability to move your legs apart
- Getting ‘stuck’ in a position and struggling to change position
The site of pain can vary. It can include the lower back, buttocks, groin, front or back of thighs, over the hips, around the pelvic floor/perineum and in the lower abdomen.
Management of pain during pregnancy
Seeking help early during pregnancy can help significantly – this may be from your GP, midwife or local physiotherapy service. Referral to local pregnancy and postnatal support and wellbeing groups can be useful or joining local pregnancy support and exercise groups. Pain medication may also be helpful.
However, general advice on maintaining good sleep, diet, hydration, and activity as well as mental self-care and relaxation are all known to help us manage and improve our pain significantly.
Remain as active as possible within the limits of pain, taking regular breaks. Exercise should feel good and maintaining your fitness and exercise during pregnancy is helpful.
Rest when necessary, as your body tires more quickly in pregnancy. Often having a rest / relaxation time for 5-10 minutes at regular intervals can help reduce strain on your body and enable you to continue through the day more easily.
Ask for help with activities that increase pain or with housework, shopping, childcare.
Plan ahead to limit extra trips up and down stairs.
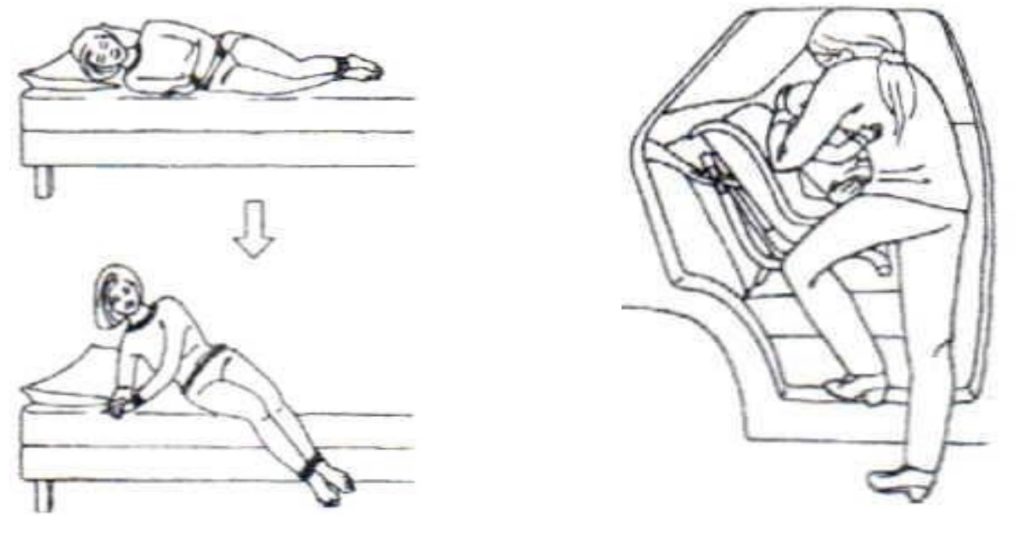
Keep your knees together when turning over (or turn under) in bed. Also, when getting in/out of a car, bed, or bath – see pictures below.
Gently exercise your tummy muscles and pelvic floor muscles regularly, and especially pull them in gently when changing position or lifting.
Wear flat supportive shoes – high heels and thin-soled shoes increase the forces going through the pelvis and spine and create more irritation.
Warmth (heat pack or warm bath/shower) or ice packs for pain relief (remember to wrap ice pack in a damp cloth before applying to the skin to prevent ice burn – use for 5-10mins max).
Try to avoid (especially if they cause pain):
- Standing on one leg (e.g. get dressed sitting down).
- Standing or sitting for long periods of time – change position regularly
- Twisting and bending to lift.
- Carrying a toddler on one hip.
- Regular heavy lifting – (i.e. using the vacuum, shopping, wet washing, heavy toddler).
- Cross legged sitting.
- Pushing heavy supermarket trolleys (use a small trolley or try online shopping).
During labour
Most women with PGP and LBP in pregnancy are able to have a normal vaginal birth. PGP is unlikely to get worse during labour and it should not affect where or how you choose to birth.
Inform the midwife that you have had pelvic or back pain, so they are aware when making your birth choices and plan. Do not put your feet up on the midwife’s hips to push.
Do:
- Use gravity to help the baby move downwards by staying as upright as you can (kneeling/standing or on all fours)
- Find a comfortable position for your pelvis using pillows to support your legs. Kneeling and leaning over a bean bag / large ball can allow you to relax and rest without any pressure on your pelvis.
- Or try side lying if you have to stay on the bed.
Following delivery
The good news is that most women find the symptoms resolve on their own after the birth, usually immediately or within 2-3 weeks.
However, if symptoms persist, continue with the advice given during pregnancy and seek advice from your GP at your post-natal check. You may need further physiotherapy and you can return to your local physiotherapy department if you had care from them during pregnancy or you can self-refer to physiotherapy.
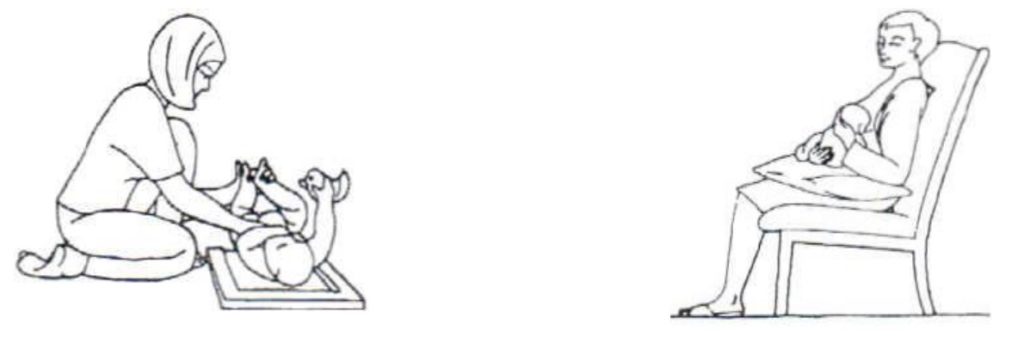
Be aware of your back and posture when feeding, changing & lifting to prevent further pain. Get baby as close to your breasts for breast-feeding with the support of pillows so that you do not need to bend forward.
It is a good idea to focus on exercises that strengthen the area around your back and pelvis following your delivery, after 6 weeks, and especially if you plan to have another pregnancy in the future. Activities such as walking and swimming are good forms of exercise and strengthening exercises such as Yoga, Pilates or gentle home exercises can be helpful.
Further information and resources
Pregnancy Related Pelvic Girdle Pain and other common conditions in pregnancy | POGP (thepogp.co.uk)
For further resources at MKUH visit: www.mkuh.nhs.uk/therapy-services/pelvic-health
