Appendicitis and Your Child
Please note, this page is printable by selecting the normal print options on your computer.
What is Appendicitis?
Appendicitis is when the appendix becomes inflamed, causing swelling and pain. The inflamed appendix becomes infected with bacteria (germs) from the intestine which then multiply quickly causing the appendix to swell and become filled with pus. If the infected appendix is not treated eventually it might perforate (burst). This can be serious as the contents of the intestine then spills into the abdominal cavity causing an infection of the abdominal membrane (peritonitis), or an abscess in the abdomen. If appendicitis is suspected it is important to start treatment early.
What and Where is the Appendix?
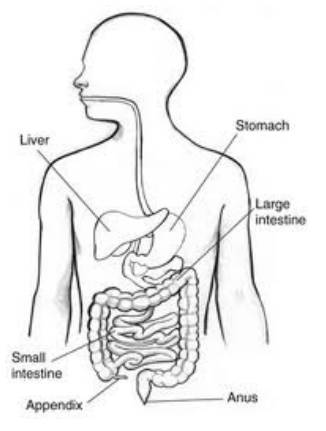
The appendix is usually located in the lower right side of your abdomen. The appendix appears to have no known function and therefore the removal of the appendix causes no health problems. The appendix is a small pouch that is located between the large and small intestine. The stomach is attached to the small intestine. This is where the food we eat is digested. The small intestine then connects to the large intestine, there the food that is unable to be digested is formed into faeces.
Symptoms of Appendicitis
• Pain in the abdomen (tummy pain). This pain commonly develops quickly starting in the middle of the abdomen and within a few hours ‘travels’ to the lower right hand side of the abdomen where the appendix is located.
• Feeling sick, loss of appetite
• Vomiting
• Fever (high temperature)
• Constipation or diarrhoea
Diagnosis
Appendicitis can be tricky to diagnose because symptoms can differ between each individual. Some people have pain that is similar to that of appendicitis but is caused by another condition. All children admitted with suspected appendicitis will have a blood test and a urine sample taken to check for any signs of infection. A doctor will examine your child’s abdomen; they may recommend an ultrasound scan to help with diagnosis. An ultrasound scan is a painless test that uses sound waves to create images of organs and structures inside the body. However there is no test that can prove the diagnosis. Sometimes the doctors will recommend waiting and observing your child’s symptoms for a day while in hospital. It is important to be aware that the surgeons cannot diagnose
appendicitis until the operation is carried out.
The uncertainty must be balanced against the risk of the appendix perforating or an unnecessary operation. If your child is admitted with suspected appendicitis, they will not be able to eat or drink (nil by mouth) until they have had a surgical review. Dependant on this review they will either be able to eat and drink small amounts or remain nil by mouth. If they are to remain nil by mouth for a long period of time they will have a drip inserted. This will give them fluid through their cannula into a vein ensuring that they are kept hydrated until after the operation. The surgeon may also start your child on antibiotics via the cannula to treat the inflammation.
Treatment
If appendicitis is suspected the treatment is surgical removal of the inflamed appendix. This is called an appendectomy. The surgical procedure will be carried out under a general anaesthetic so your child will be asleep.
There are two methods in which an appendectomy is carried out:
• Laparoscopic appendectomy- involves 3 very small incisions into the lower abdomen where a laparoscope and camera are passed into the abdomen to remove the appendix. These small incisions are often closed with glue or dissolvable stitches.
• Open appendectomy – involves 1 small incision usually around 6-8cm in length to the right of the abdomen. The appendix is then removed from the surrounding organs. The incision is closed with dissolvable or removable stitches.
Sometimes children will go to theatre for a laparoscopic appendectomy however in theatre this may change. Should this occur the surgeon will explain why this decision was made.
Care After Surgery
When your child returns to the ward they will be quite sleepy. They may still have their drip running until they wake and are able to drink normally. Your child may feel some discomfort around the incision site. Medication can help reduce this so make sure your nurse is aware if they are uncomfortable. The surgeon will have made a plan of your child’s postoperative care dependent on whether the appendix was inflamed or had burst. If the appendix had burst the intestine takes a bit longer to recover from the surgery and it may take a little longer for your child to be able to eat
and drink. A good indication the gut is beginning to work normally is that your child will begin to pass wind.
Once your child is eating and drinking small amounts and are able to mobilise they will hopefully be ready to be discharged home. The length in hospital stay can vary dependant on recovery time. Most children will stay between two and three days. However if the appendix had burst then the length of stay could be up to seven days as they may need a longer course of antibiotics. Sometimes children are discharged home on oral antibiotics. Prior to your child’s discharge the wound dressing should be changed. The wound site may be slightly pink but should be clean and dry.
On Discharge
Most children’s wounds will have been closed using dissolvable internal stitches, or glue. However sometimes they may have stitches that need to be removed. The community children’s nurses will contact you to arrange to remove the stitches usually around 7 days post-surgery. It is OK for your child to wash. However the wound should not be soaked. It is advised that they should shower or have a very shallow bath, not submerging the incision site, and just dab the site dry. Do NOT rub while the wound is healing.
In many cases your child will be able to return to school within a week of surgery. However, if it had burst this may take a bit longer. It is advised that they avoid any vigorous exercise or swimming until the wound has fully healed and should avoid all contact sport for 6 weeks.
When to be concerned
• If your child develops a fever.
• If the wound site becomes red, hot or swollen.
• If the wound starts to discharge/ooze.
• If your child’s tummy becomes distended (starts to swell).
• If you do not think that they are recovering as you would expect.
If any of the signs above take place you should contact your GP to ask for them to be seen or contact our community children’s nurse team for advice.
