Anterior Resection
Please note, this page is printable by selecting the normal print options on your computer.
Introduction
Anterior resection is the name given to the operation to remove the diseased part of your bowel. The operation can be done in two ways:
- It can either be performed in the traditional method of opening up the tummy from above your navel (tummy button) down in a straight line (approximately twenty centimetres in length). The wound will either be stitched, stapled or glued back together at the end of the operation and will heal in ten to fourteen days in an uncomplicated case.
- Or the operation can be performed laparoscopically. The other names for laparoscopic surgery are keyhole surgery, minimal access surgery or minimally invasive surgery.
A laparoscope is a thin telescope with a light source. The laparoscope is passed into the abdomen through a small incision (cut) in the skin often referred to as a port. It is used to light up and magnify the structures inside the abdomen. This is then connected to a television monitor for the surgeon to see more clearly. Fine instruments are then passed into the abdomen through three or four small incisions in the skin. These instruments are used to lift, cut and take a biopsy from inside the abdomen.
The decision of which method is used to perform your operation will always be made with your best interests in mind and discussed with you. However, occasionally it is necessary to abandon laparoscopic surgery and open up the abdomen, if it becomes difficult to proceed safely with laparoscopic surgery.
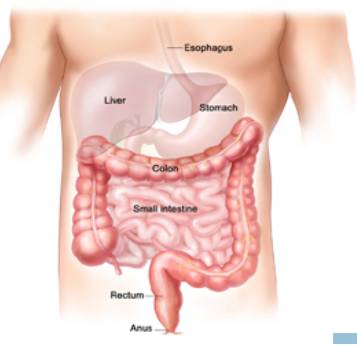
The Large Bowel
The large bowel (intestine or colon) is approximately 1.5 metres long. This part of the digestive tract carries the waste from digested food from the small bowel and gets rid of it as waste through the opening in the back passage (anus). Cells that line the bowel may begin to grow abnormally, forming a tumour (a growth of cancer cells). Tumours start in the lining of the bowel and can grow through some or all of the other layers.
Treatment Options
Bowel cancer can be treated in a number of ways, with people often having a combination of treatments. Your treatment will be designed to your individual needs.
- Anterior resection which is the operation described in this leaflet
- Radiotherapy is used for some people as the initial treatment for cancer in the rectum (back passage). This is to shrink the tumour and make it easier to remove with an operation.
- Short course radiotherapy (over 5 days) is done specifically to reduce the chance of the cancer coming back.
- Long Course radiotherapy (daily for 5 weeks) is done specifically to reduce the size of the cancer.
- Chemotherapy (use of drugs to treat the tumour) is sometimes used either before or after surgical removal of the cancer.
- Placement of a stent, which is a wire mesh used to stop the bowel from blocking (this is only suitable for cancers in certain parts of the large bowel).
Anterior Resection
Removal of the diseased part of the bowel by an operation is the best treatment for a tumour of the bowel. The aim is to give you the best chance of a cure through total removal of the tumour. This operation is usually done to remove a tumour in the upper or middle part of the rectum (back passage) although it can be performed for other reasons as well.
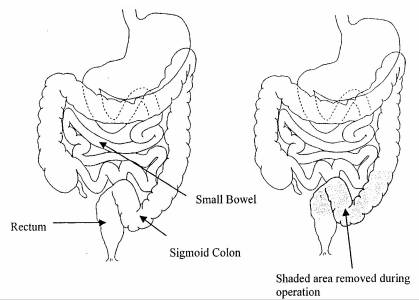
The cut ends of the bowel are then re-joined together. This new join is called an anastomosis. Sometimes the join will need longer than a few days to heal. In that situation, your surgeon would make an opening into the small bowel called an ileostomy (stoma). There is a higher chance of having a temporary ileostomy if the new join in the bowel is very low. The ileostomy would then be closed at a second operation.
Diagram of an ileostomy:
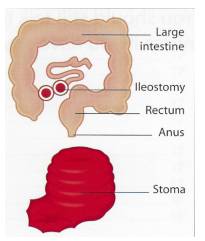
The ileostomy (stoma) drains the waste from the bowel into a stoma bag; the waste from the bowel is more liquid than normal bowel waste from your bottom.
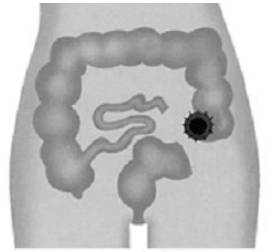
If you have an ileostomy you will see the specialist stoma nurse for help and advice and she will also give you written information about the ileostomy. If you would like more information about an ileostomy before your operation please contact the stoma nurse on 01908 660033 and ask for extension 86951. Occasionally, it is not possible to re-join the bowel at the time of the operation and the bowel is brought out onto the surface of the skin as a colostomy (stoma). The colostomy allows the waste from the body to pass out through the abdomen into a stoma bag.
The waste from this part of the bowel is very similar to the waste from your bottom. If you have a colostomy, you will see the stoma nurse specialist for help and advice and she will give you written information about the colostomy. If you would like more information about a colostomy before your operation please contact the Stoma Nurse on 01908 660033 and ask for extension 3070.
Diagram of colostomy:
Risks of this operation
Any operation carries a risk, the risks of all operations include:
- Chest Infection. This would require antibiotics and physiotherapy
- Blood Clots in the legs (deep vein thrombosis) or in the lung (pulmonary embolism). We decrease this risk by using elastic stockings and blood thinning injections.
- Anaesthetic – this operation is carried out under a general anaesthetic (you will be asleep). If you would like an explanation sheet about general anaesthetics and the associated risks please ask for one. If you are at increased risk because of other medical problems you may have your consultant will refer you to an anaesthetist for a formal assessment.
- Bleeding. This can occur with any operation.
- Patients who are very overweight, smoke or have other medical problems are at increased risk of all of these complications.
- Compartment Syndrome – Compartment syndrome is a rare but painful and potentially serious condition caused by bleeding or swelling to an enclosed space within the muscles. The pressure within the space can increase to such an extent that it affects the function of the muscle and nerves. The area most likely affected with the operation you are having is the legs, this is due to the position your legs have to be in during the operation, however it can affect your arms, tummy or the cheeks of your bottom. Pain is the most common symptom followed by numbness. The treatment is an operation called a fasciotomy.
The surgeon would need to open the skin and muscle of the area affected to relieve the pressure and prevent permanent damage. The wound is dressed but is not closed with stitches until approximately 48-72 hours later. You may not be allowed to get out of bed and weight bare until the wound has been closed. This is a major operation that has serious risks of which a small number of people do not survive. Your consultant will discuss your individual risks with you and answer any questions you have. Measures are taken to reduce these risks; however it is not possible to stop all risks completely.
The risks of this operation also include:
- Leakage where the bowel was stitched together. This occurs in around 5% of cases but is a serious complication. It is treated with antibiotics and often requires further surgery which usually results in a stoma (as previously mentioned).
- Pelvic Nerve Damage – there is a specific risk of damage to the nerves of the pelvis which supply control to the bladder and sexual organs. In a man this can lead to impotence (failure to have or maintain an erection or ejaculate). In a woman it can cause painful intercourse. In both men and women the bladder can be affected making it difficult to pass urine.
- Increased risk of infection – because the bowel is an organ that is full of bacteria. This may be in the form of a wound infection or an infection inside the abdomen in the form of an abscess. Antibiotics are given to help control the infection and sometimes drainage of an abscess is necessary.
- Bowel stops working. This is temporary but can cause bloating of the tummy and sickness
Risks of not having the surgery
Just as there are risks of having surgery there are also risks of not having surgery. These include:
- Symptoms such as pain and bleeding may become worse.
- The bowel could become completely blocked or even burst which could lead to further complications and may need surgery.
- The cancer could also spread to other parts of your body.
Preparation for Surgery
You will also be given an enema into your bottom to ensure your bowel is empty approximately 2 hours before your operation. The stoma nurse will see you at this point and discuss with you where the stoma would be placed on your tummy if it was necessary. It is important to mark this position with a pen to make sure the stoma would be placed in a suitable position for you to manage.
If you have been told you are to follow the enhanced recovery programme please read the enhanced recovery information sheet. Enhanced recovery is a way of preparing you for surgery so that your stay in hospital is as short as possible.
After Surgery
The recovery period after bowel surgery varies. It usually involves a stay in hospital from three to ten days (in uncomplicated cases) depending on whether you had open or laparoscopic surgery. Immediately after your operation the following tubes may be in place to help us care for you:
- Pain control will be administered through either an epidural (tube into your back) or a drip (tube into the veins on your arm). This will help you move around more freely. As you recover these will be removed and pain killers will be given in the form of tablets. The pain gradually eases, particularly once you are up and moving around
- Fluids in the form of a drip in your arm will keep you hydrated until you are able to drink freely
- A catheter (tube to your bladder) will drain your urine into a collection bag so we can accurately measure the amount
- A drain into your tummy-this is a tube to drain fluid away from the area where the bowel has been joined. This will be removed when it finishes draining usually within two to five days.
These tubes are removed as soon as possible depending on your recovery. The nursing staff will help you get you out of bed as soon as possible after the operation to reduce the risk of complications from the operation.
Diet
You may be able to eat during the first few days of recovery but your appetite will probably be reduced. It is important to eat small frequent amounts of easily digested food. In the initial few days you will be given specific advice on what you can eat. Meals can be supplemented with nourishing soups and snacks and high energy drinks. The body requires lots of calories during the healing process. After the first few days there is no special diet and we encourage you to build up to your normal diet as soon as you can tolerate it. There is no special diet after this operation and we
encourage you to build up to your normal diet as soon as you can tolerate it.
If you have an ileostomy, the stoma nurse will give you detailed dietary advice. If you have a colostomy you may follow a normal diet.
Bowel actions
The bowel may take a little while to recover and the sensation that you need to go to the toilet can be different. This is usually temporary but can take some time to settle down. Passing wind is a sign that your bowel is starting to work again. It is normal for the bowel to be irregular and sometimes is necessary to give medications to either slow the bowel down or give mild laxatives to encourage the bowel to move (even if you have a colostomy).
If you have an ileostomy the stoma nurse will give you advice on how much output is normal and how to help reduce the amount if necessary.
Exercise
You will be encouraged to get out of bed the following day and you will be seen by a physiotherapist who will help you do this. You will be wearing elastic stockings to reduce your risk of a blood clot but moving around will also help. The physiotherapist will also give you deep breathing exercises as this will help prevent chest infections. Lifting after abdominal surgery is not recommended for approximately four weeks after your operation. If you have a stoma, the stoma nurse will give you detailed advice on lifting.
Stoma Care
If you had a stoma formed during your surgery (either a colostomy or an ileostomy), the stoma nurse specialist will see you regularly to give you help and advice on managing your stoma and you will be given all the equipment you need to do this. You have to be able to manage your stoma with out help before you can be discharged home. The stoma nurse will also visit you at home within a few days after discharge to monitor your progress.
Driving
Check with your insurance company about any exclusion they may have. This includes being under the influence of some pain medication. You must be able to perform an emergency stop and you are not excluded from wearing a seat belt.
When you go home
When you go home you may find that on some days you feel better than on other days. It is quite normal to have ‘good’ and ‘not so good’ days. However, it is important to contact the GP if any of the following occur:
- Discharge or leakage from the wound or drain site
- High temperature
- Uncontrolled shivering/ feeling hot then cold
- Pain when passing urine / frequent need to pass urine or very offensive smelling urine
- Difficulty with breathing, chestiness or cough with green or yellow phlegm
- Pain in the calf, leg or chest
- Abdominal pain which is different from the usual post operative soreness
- Bleeding from the back passage
- Vomiting
Results of your Operation
The piece of bowel that is removed is sent to the laboratory for detailed testing. The results will take ten to twenty days to be processed and a report will be sent to your consultant. These results will be used to determine if you need any further treatment. Your consultant or nurse specialist will then arrange an appointment to discuss with you the results.
Confidentiality
As part of your treatment some kind of photographic record may be made. For example, photographs or video. You will always be told if this is going to happen. The photograph or video will be kept with your notes and will be held in confidence as part of your medical record. This means that it will only be seen by those involved in providing care for you or by those needing to check the quality of care you have received.
The use of photographs and video is also extremely important for other NHS work, such as teaching or medical research. If we would like to use the information for these purposes we would only do so with your permission. We do not use any information in a way that identifies you.
This information leaflet is to support and not to replace discussion between you and your specialist. Before you give your consent to any treatment you should raise any questions you have with your specialist Colorectal Cancer Nurse Specialist 01908 996953. Stoma Care Nurse Specialist 01908 243070. Please leave a message on our answer machine if we are not in the office.
