Percutaneous Endoscopic Gastrostomy (PEG) – Information and Care Guidelines for patients and carers
Please note, this page is printable by selecting the normal print options on your computer.
Introduction
This booklet aims to provide you with information about your PEG tube.
It explains what the procedure is, how it is performed, and gives aftercare advice. If you have additional questions, please contact your Nurse or Dietitian who will be able to help you.
What is a Percutaneous Endoscopic Gastrostomy? (PEG)
- Percutaneous – meaning something is inserted through the skin
- Endoscopic – the instrument used to place the PEG tube is called an endoscope
- Gastrostomy – means an opening into the stomach
A PEG is a small tube that is inserted through the skin directly into the stomach so that you can receive feed, water and medication.
What does a PEG look like?

Freka ®PEG
Why do I need a PEG?
You are unable to take enough food and fluid by mouth to meet all your nutritional and hydration needs. The PEG can help to meet these requirements as feed and fluid can be given directly into the stomach.
How long will I be in hospital?
If you are an outpatient, you will normally be admitted to a ward the day before the procedure. If you are not going to be using the PEG for feed straight away, you should be able to go home the day after the procedure.
If you need to use the PEG for feed and medications immediately, you will need to stay in hospital a few days longer so that the feeding regimen can be established.
How long will the tube last?
The PEG tube is made from polyurethane and if it is well cared for it can last for several years. Depending on the reason that you are having the PEG, you may only need it for a short period and then it can be removed.
Where will the procedure take place and how long does it take?
The procedure takes place in the Endoscopy Department, and it takes approximately 30 minutes.
Can I still eat and drink after the PEG is placed?
You may be able to eat and drink, but this depends on the reason why you are having the PEG tube inserted in the first place.
If you are having swallowing difficulties the Doctor may refer you to a Speech and Language Therapist who will be able to advise you on what you can safely eat and drink.
What are the risks and possible complications?
PEG placement is generally a safe and well tolerated procedure. However, the following are potential risks:
- Reactions to the medication given (sedative)
- Infection at the insertion site.
- Bleeding from the incision site.
- Perforation, which is a little tear in the wall of the bowel. This is rare and would require a hospital stay for antibiotics and possibly a surgical repair.
How do I prepare?
- If you are diabetic, it is important that you contact your diabetic nurse or assessment nurse prior to any of these preparations so that they can instruct you on what you need to do.
- If you are taking any medicines e.g. Warfarin, Aspirin or Clopidogrel these may need to be altered or stopped before your procedure. You may also need to have blood tests. Please speak to your GP, the assessment nurse, or the hospital doctor for advice.
- Before the procedure it is important that your stomach is empty. Please do not eat or drink anything for at least six hours (preferably overnight) before the procedure.
- If you have a nasogastric tube as a method of feeding you should not have any feed through it for at least six hours (preferably overnight) before the procedure.
What to bring with into hospital with you?
- Your appointment letter and the health questionnaire. Please complete the health questionnaire.
- A dressing gown and a pair of slippers.
What happens when you arrive on the ward?
- On arrival, a member of the medical team or the nutrition nurse will discuss the procedure with you.
- Some blood tests may be taken and a small intravenous cannula will be placed into a vein in your hand or arm.
- You will be referred to the dietitian.
When you arrive at the Endoscopy department:
- You should not have had anything to eat or drink for 6 hours prior to the procedure.
- The nurse will ask whether you have any allergies to any medicines, any medical conditions and anything which may require you to be given additional antibiotics before the procedure (for example an artificial heart valve or if you suffer from valvular heart disease).
- They will ask you for details of any medicines you are currently taking, e.g. Warfarin, Aspirin and Clopidogrel. It is important that the doctor in the Endoscopy department is aware of these and any other conditions before the procedure is started.
- Before you go to the endoscopy room, the Doctor or Nurse placing the PEG will discuss the procedure, explaining any risks and give you the opportunity to ask questions. Then you will be asked to sign a consent form. This will be completed before you go to the endoscopy room.
- In the endoscopy room you will be asked to lie on your back. You will be administered sedation (this is usually a sedative called Midazolam).
- Your throat may be made numb by using a local anaesthetic spray and then a flexible tube (endoscope) will be passed through your mouth into the stomach. This will allow the doctor to inspect your stomach and identify the correct position for the PEG.
- Once the PEG is inserted a dressing is applied and you will be transferred back to the ward.
What happens after the procedure?
- Do not eat or drink anything for 4 hours after the procedure and remain on bed rest for 4 hours.
- You will be given fluids through the cannula to prevent you from getting dehydrated.
- The ward nurses will monitor your observations such as blood pressure and heart rate and ask if you have pain at regular intervals. When the PEG is first placed, it can feel uncomfortable and so you may require regular pain relief which will be prescribed.
- Nothing should be put through the PEG for 4 hours after the procedure.
- After 4 hours, the nurses will commence an infusion of water, which will run for 6 hours.
- If there have been no complications with the water infusion, enteral feeding and medication can be given via the PEG the following day from 8am.
Starting to feed through the PEG
If you need to start feeding through the PEG straight away, the dietitian will see you the day after placement to prescribe a feeding regimen. There are two ways of feeding:
- Using a pump to deliver the liquid feed slowly throughout the day
- Bolus feeding- liquid feed is drawn up into a purple 60ml syringe and then slowly given directly through the PEG.
The dietitian will help you to decide the most suitable method for you. You will need to stay in hospital until the feeding regimen has been established and training on how to give the feed has been provided to you and/or your carer/s.
If I do not need to use the PEG straight away for feed, do I need to do anything with the tube?
Yes, the PEG will need to be flushed twice daily with 50mls of water to keep the tube clear. The nutrition nurse or the ward nurses will show you how to do this before you go home.
Before discharge from hospital, you should be provided with the following.
- 10 packets of sterile gauze and 10 sachets of normasol for cleaning around the PEG for the first 10 days.
- Tape for securing the tube to the abdominal wall.
- 14 days’ supply of feed and the equipment required to give the feed/water flushes.
- The contact details for the Abbott Nutrition Nurse.
Following discharge
If you are discharged within 24 hours of having sedation do not:
- Drive a car or ride a bike
- Drink alcohol
- Operate any machinery or do anything requiring skill or judgement
- Make important decisions or sign documents
Important Notice:
If you are discharged within 72 hours of having your PEG placed and you notice any of the following symptoms, DO NOT PUT anything through the PEG and contact Ward 22 on 01908 996455/996454 or go to Accident and Emergency URGENTLY:
- Leakage of fluid around the PEG tube.
- Pain on feeding or flushing with water (stop the feed).
- Prolonged or severe pain with possible abdominal bloating.
- New bleeding from the PEG site.
Looking after your PEG at home
- Always wash your hands thoroughly before touching the PEG and the insertion site.
- Clean around the PEG tube site once daily for the first 10 days with saline/normasol and sterile gauze. After this time clean with mild soapy water and dry well.
- Leave the feeding line clamp open when the PEG is not being used for feeding, as this will prevent flattening of the tube.
- The feeding tube should be flushed with at least 30mls of water before and after feed or medicine administration. This will prevent the tube from blocking.
- It is advisable to tape the end of the PEG to your abdomen to prevent it from pulling.
- You can take a shower after 48 hours but do not take a bath for two weeks or until the site has healed.
- If the insertion site is painful or red the nurse or the GP will take a swab to check for infection.
- In the rare event that your PEG falls out it is essential that you act quickly before the tract closes. Go to A&E immediately and they will contact the appropriate team.
Medication
If possible, medications should be taken orally. If you cannot take medication orally then your tablets may be able to be crushed, mixed with water and given through the PEG.
Note: Not all medications are suitable for crushing and putting through the PEG. Some tablets are available as a liquid, which is easier to give through the PEG. If you are unsure, please discuss with your GP or pharmacist.
It is important that the medications are given separately and not mixed. Always flush the PEG with at least 30mls of water in between each medication.
What do I do if the PEG blocks?
If you are unable to flush the tube, you may try the following:
- Ensure all clamps are open and the tube is not kinked.
- Put 30mls of water into a 60ml purple syringe and try to clear the tube using a gentle push/pull technique on the syringe.
- If this does not work, try using warm water. Do not use fizzy drinks.
- If the blockage still does not clear, contact your Abbott nutrition nurse.
- Out of hours, please come to the Accident and Emergency department.
- Never use a sharp instrument or excessive force to clear the blockage.
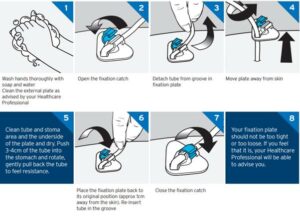
Rotating and advancing the PEG
To prevent the internal bumper of the PEG from becoming buried it is very important that the PEG is advanced and rotated daily. This should start 10 days after placement and not before. The Abbott Nutrition Nurse will be informed of your discharge and asked to visit to support you with the first advance and rotation of the PEG.
Courtesy of Fresenius kabi
PEG Replacement and Removal:
If your PEG needs replacing, your GP may refer you to the hospital to be seen by the Gastroenterologist and the Nutrition Nurse. They will review the PEG and decide if it needs changing. If you no longer need your PEG, your GP will refer you to the Gastroenterologist to remove it.
Useful Contacts:
Community Dietitian: 01908 995416
Community Abbott Nutrition Nurses: 07824483335
Hospital Nutrition Nurse: 01908 660033 ext. 87397 or 87398
