Diabetes Insulin and exercise
Please note, this page is printable by selecting the normal print options on your computer.
Everyone should be encouraged to exercise, and having diabetes should not stop you from taking up an activity or exercise you enjoy. All exercise will cause an increase in the uptake of glucose by your muscles. In other words, exercise lowers your blood glucose level. In diabetes there are difficulties with the balance of hormones. Injected insulin levels and fluctuating adrenaline levels together increase the likelihood of experiencing hypoglycaemia (low blood glucose) either during or up to 24 hours after activity.
New research has shown that some people may find that during vigorous exercise, for example sprinting, blood glucose levels actually increase as the activity is very intense and adrenaline rises. If this applies, you may want to discuss this with your diabetes team. To reduce the chances of hypoglycaemia (hypo) happening, you need to plan ahead where possible and alter your carbohydrate intake and/or insulin intake, eat more carbohydrate or take less insulin. With planned activity you have this option. If you are trying to lose weight, it is probably best to reduce your insulin
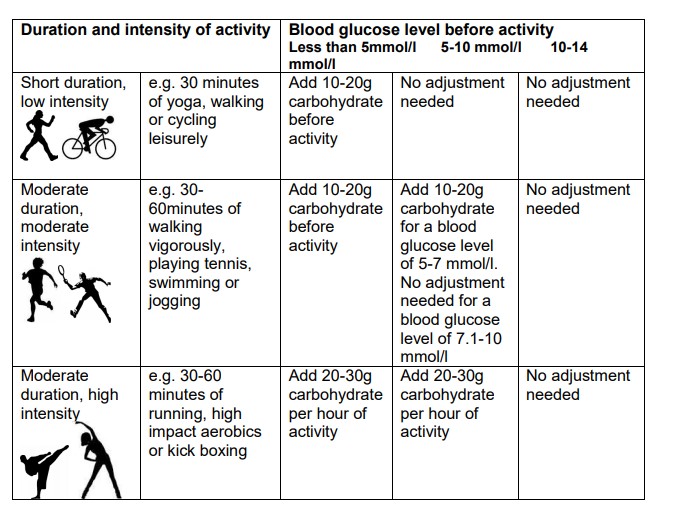
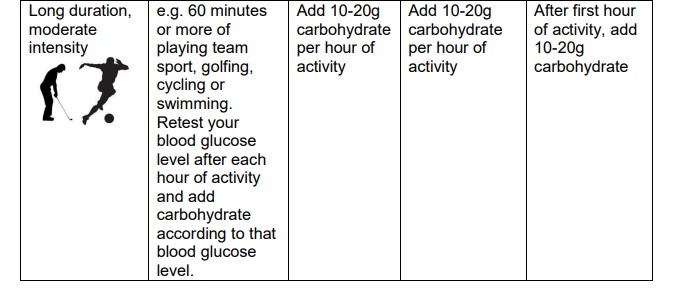
in advance. Speak to your diabetes team for guidance on how to do this. If, however you are doing unplanned exercise, you will have to have more carbohydrate (see table on page 3 for more information on this).
The current guidelines for physical activity are 150minutes of moderate activity or 75 minutes of vigorous activity over a week. The activity can be in bouts of 10 minutes or more.
High blood glucose levels before activity
– Be careful when your diabetes is poorly controlled or your blood glucose level is more than 14 mmol/l. Activity, in this situation, can raise your blood glucose level rather than lower it. If this happens, it is because you may not have enough insulin circulating in the body. Consider injecting an extra dose of bolus insulin (correction dose) and, if you have type 1 diabetes, always check for ketones (the by-product of the body breaking down fat for energy). If ketones are present, you need to avoid doing any activity until your ketones have gone.
Checklist to avoid problems during or following physical activity:
– Test your blood glucose levels more often, particularly before, during and hourly after activity. This will help you understand your body’s response.
– If ketones are present with high blood glucose levels (more than 14 mmol/l), delay exercise until you have got rid of the ketones, as this could lead to ketoacidosis (dangerous complication caused by a lack of insulin in the body).
– If blood glucose levels are below 5 mmol/l before the activity, take additional carbohydrate, without matching it to a dose of insulin.
– If you have blood glucose levels of less than 4 mmol/l, you are having a hypo. Make sure you treat this appropriately.
– Be prepared to decrease your insulin, increase your carbohydrate intake or both.
– After exercise carbohydrate needs to be taken again to replenish muscle and liver stores of glucose. Typically, 1.5 grams of carbohydrate per kilogram of body weight, taken with bolus insulin.
– Be aware that absorption of insulin may be faster if you inject into a limb that will be used for activity, such as your leg if you are running or arm if you are swimming – Always carry hypo treatment.
– Make sure you drink plenty of fluids during prolonged activity.
– If being active alone, make sure someone knows where you have gone.
– Teach those with you on how to help in the event of a hypo.
Unplanned activity
The table on page 3 is a guide to show how you might adjust your carbohydrate intake when taking part in unplanned physical activity.