Last Modified: 10:35am 22/04/2020
Intensive Care for Coronavirus patients at MKUH
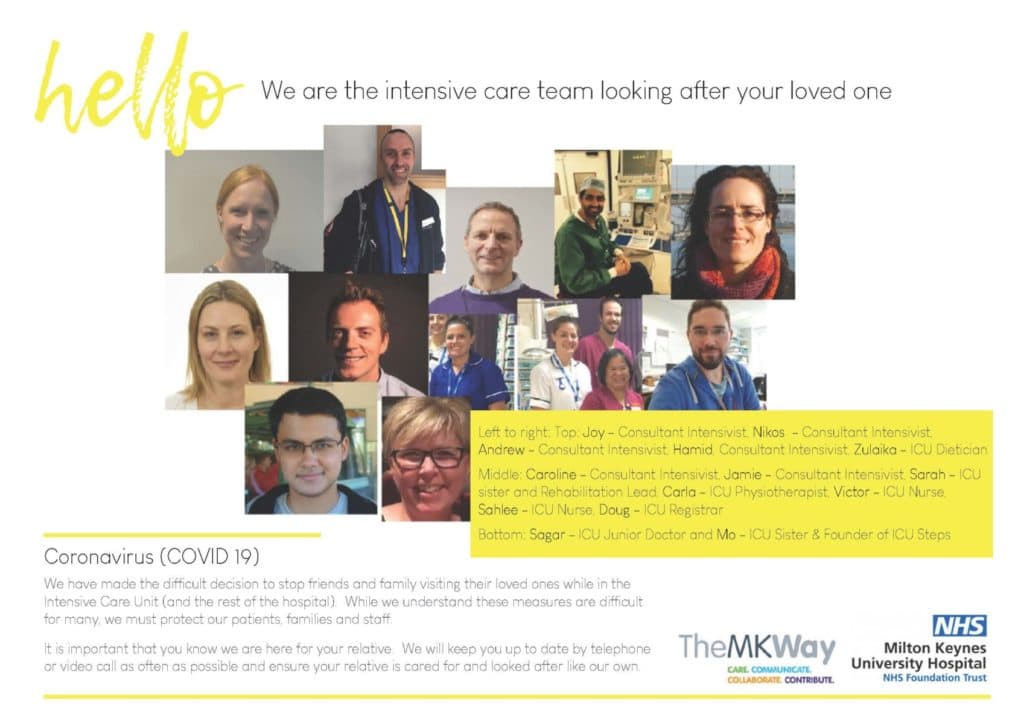
The Staff
While we understand the visiting of loved ones being stopped is difficult for many, we must protect our patients, families and staff. However, it is important that you know who is looking after your relative, so please see our ICU staff poster.
What is Coronavirus (COVID-19)?
COVID-19 is the name of the disease caused by the novel coronavirus. This virus is a member of a large family of viruses, including those that cause the common cold. Common symptoms of COVID-19 include fever, cough and shortness of breath. This novel version of coronavirus appears to affect some people more severely. Some people require treatment in hospital, some require more intensive support in an intensive care unit, and some people unfortunately may not survive.
How is COVID-19 treated in hospital?
Unfortunately there is no cure for COVID-19.
Treatments are aimed at supporting patients’ breathing and circulation and include:
- Oxygen therapy to help make breathing easier and improve the function of body organs
- Fluids
- Drugs to reduce fever
If patients require more support than this, then they may require admission to the intensive care unit
Why is my relative in ICU?
Your relative has been admitted to the intensive care unit because they require specialised treatment, monitoring and interventions. In the case of Coronavirus, it is most likely that your relative needs more help with breathing and delivering oxygen to their blood using advanced breathing equipment that we have on the intensive care unit.
These patients have a nurse allocated to care for them 24hrs a day, as well as a team of doctors who attends to them throughout the day and night.
We want you to know that we understand the pain and anguish that you are going through in these difficult times. We appreciate how hard it is that you cannot see your loved ones and be at their bedside. We want to let you know that your relative will be cared for and cherished in our intensive care. They will be spoken to, soothed & comforted even if asleep on a ventilator.
What are the different ICU1 and ICU2 at Milton Keynes University Hospital?
Due to the Coronavirus crisis, more patients than usual are being admitted to intensive care units nationally. We have expanded the number of intensive care beds in the hospital to offer the best support to patients.
Milton Keynes Hospital now has two intensive care units. These are called ICU1 and ICU2.
ICU1 is the original intensive care unit whereas ICU2 is located next to the phase 2 operating theatres.
Both these ICUs provide the same level of support, staffing and equipment to care for your relative.
What happens on intensive care during this Coronavirus crisis?
 (This patient consented to photos/videos. We have chosen to protect his identity)
(This patient consented to photos/videos. We have chosen to protect his identity)
The Intensive Care team includes a wide range of health care professionals working together to deliver expert care. On intensive care, patients are cared for by a team of nurses, doctors, physiotherapists and healthcare support workers. The Intensive Care team work closely with specialist pharmacists, dieticians, radiographers and doctors in other specialties including infectious diseases and respiratory medicine.
The members of the ICU team work together around the clock to provide treatment. They will closely monitor your family member’s condition and review their treatment regularly to see if it is making a difference. We hope that if treatment is successful they will recover to return to a quality of life that is acceptable to them. However, after intensive care treatment, your family member will almost certainly not be as fit as they were. This is even more likely if they are already frail or have other illnesses.
At least two ward rounds happen on ICU each day, one in the morning, and one in the late afternoon. During these ward rounds the nurses, doctors and other team members will review all relevant information about a patient’s status and progress and make decisions about changing or adding certain treatments. The doctors and nurses are present all day and all night and are able to respond to any changes in a patient’s condition.
Treatments are tailored to each individual patient. Some treatments are listed below. Not all of these treatments may be required, and other treatments that are not listed here may be used.
· Non-invasive ventilation
This is sometimes referred to as CPAP, BiPAP or mask ventilation. This is a way of helping patients to breathe more deeply by blowing extra air into the lungs via a mask when they breathe in.
· Invasive ventilation or mechanical ventilation
A mechanical ventilator (breathing machine) is a machine that helps a patient breathe. It is used in patients who require more help to breathe than with oxygen or non-invasive ventilation. The patient is connected to the ventilator with a hollow tube (called an endotracheal tube) that goes in their mouth and down into their main airway or trachea. This can be uncomfortable and therefore patients are sedated with medication to keep them comfortable.
· Renal replacement therapy
This is a form of temporary dialysis which helps to remove toxins from the body.
· Medicines to support blood pressure
Medications can be given to help the heart deliver blood to other organs more effectively.
· Proning
Patients may be re-positioned on to their fronts. This may improve their breathing.
· Feeding
Some patients may not be able to eat and drink normally. Nutrition will be delivered either by a small tube that passes from their nose in to their stomach (nasogastric tube), or via a drip.
· Antibiotics
Antibiotics do not treat COVID-19. However, patients may require antibiotics if they have an additional type of infection.
· Support and Care
Patients are always treated with respect and compassion, and our staff are working hard to provide emotional support to patients in this particularly difficult time with reduced family visiting.
· Research studies
COVID-19 is a new disease and new treatments may be trialled in the intensive care unit to help improve care.
Communication
Why can’t I visit?
We have made the difficult decision to stop friends and family visiting their loved ones while in the Intensive Care Unit (and the rest of the hospital). While we understand these measures are difficult for many, we must protect our patients, their families and our staff from risk of infection.
Daily updates
Please identify a main contact within your family who will be able to pass on information to other family members. Please phone the intensive care and ask if anybody is available to give you an update. If we don’t hear from you we will also try to contact you by telephone however please bear with us if this doesn’t always happen.
Video calls
Some patients may be able to video-call you themselves via their own phones. However, communication may be challenging if patients are breathless or on oxygen therapy. If patients are on a ventilator, they are unlikely to able to communicate. If your relative has previously given us their consent before being sedated, our team can discuss the option of a video call so you can see your relative, using a safe technology called NYE Health – https://www.meet.nye.health/for-patients .
Emergency communication
A senior member of the team caring for your relative will contact the main contact in your family if there is a sudden change in your relative’s condition.
Personal calls
You can also stay in touch with your loved one in hospital via telephone (their own mobile phone, or possibly one that has been lent to them by the hospital), Skype, FaceTime or other ways of having video calls. It is important for you to know that sometimes people in intensive care become confused and disorientated. At that time they may say things that are unusual or out of character. They may become confused about the things you are trying to talk to them about. This is not uncommon in critically unwell patients and the intensive care staff are accustomed to helping patients with these temporary states of mind.
End of life care
Unfortunately, we know that a number of patients in intensive care will not recover and may die. Our dedicated palliative care team helps us to ensure that patients who we identify as being in the last days of life, are comfortable and supported
Useful contacts –
- Chaplaincy team
Chaplains are here for patients and families of all faiths and none. The Chapel is available for anyone to sit quietly or to pray. There is a dedicated Muslim prayer area with separate prayer spaces for men and women. For support please contact Lead Chaplain, Sarah Crane or Chaplain Administrator, Christine Buttery. They are usually on-site Monday to Friday 08:00 – 16:00 and Sunday morning.
- ICUSteps: An Intensive Care Support Charity which provides information and support for people who have been affected by critical illness, whether as patients or relatives ,you may find useful information that will answer some of your questions and worries in more depth. icusteps.org
- HealthUnlocked Online Support Group –https://healthunlocked.com/icusteps
Information on Covid-19 or critical care –
- The facts: clear government information about Covid-19 gov.uk/coronavirus
- Health advice and facts about Covid-19 from the NHS nhs.uk/conditions/coronavirus-covid-19
- Information to help people affected by Covid-19 make advance decisions about care criticalcarenice.org.uk/patient-information
