Care of a third-or fourth-degree tear that occurred during childbirth
Please note, this page is printable by selecting the normal print options on your computer.
About this information
In the UK, a third- or fourth-degree tear (also known as obstetric anal sphincter injury – OASI) occurs in about 3 in 100 women having a vaginal birth. It is more common with a first vaginal birth, occurring in 6 in 100 women, compared with 2 in 100 women who have previously had a vaginal birth.
This information is for you if you have had an OASI during childbirth, or if you are a relative or friend of someone who is in this situation.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
A glossary of medical terms is available on the RCOG website at: www.rcog.org.uk/en/patients/medical-terms.
Key points
- A third- or fourth-degree tear is where a tear in your perineum extends into the anus (back passage). Your perineum is the area between the vaginal opening and the anus.
- Everyone is different and recovery from a third- or fourth-degree tear will vary. You may experience pain or discomfort that can affect your mobility while you are recovering.
- There is additional support for women who feel that their mental health has been affected by their birth experience, or the effects of a tear. Talk to your healthcare professional about what is available.
- 6–8 in 10 women with a third- or fourth-degree tear will have no longlasting complications after it has been repaired and given time to heal.
- A small number of women will experience difficulty in controlling their bowels or holding in wind. This is called anal incontinence.
- There is specialist treatment available for women with anal incontinence, in the form of physiotherapy or surgery.
What is a perineal tear?
Many women experience tears during childbirth as the baby stretches the vagina and perineum. Small, skindeep tears are known as first-degree tears and usually heal naturally. Tears that are deeper and affect the muscle of the perineum are known as second-degree tears. These usually require stitches.
What is an episiotomy?
An episiotomy is a cut made by a healthcare professional through the vaginal wall and perineum. This may be done if your baby needs to be born more quickly or to make more space for your baby to be born. It is possible for an episiotomy to extend and become a deeper tear.
What is a third- or fourth-degree tear?
A third-degree tear is a tear that extends into the muscle that controls the anus (the anal sphincter). If the tear extends further into the lining of the anus or rectum it is known as a fourth-degree tear.
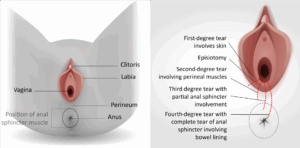
The image on the left shows a perineum without tears. The image on the right shows where the different types of tears occur.
What is a rectal buttonhole?
This is a rare injury and occurs when the anal sphincter is not torn, but there is a hole between the back passage and the vagina. This means that wind and faeces may be passed through the vagina instead of via the anus. This is not normal, and if you experience this you should see your healthcare professional urgently.
What happens if I have a third- or fourth-degree tear?
If a third-degree tear, fourth-degree tear or isolated rectal buttonhole is suspected or confirmed, this will usually be repaired in the operating theatre as soon as possible after your baby is born. You will need an epidural or a spinal anaesthetic (rarely, a general anaesthetic may be necessary). You may need a drip in your arm to give you fluids until you feel able to eat and drink. You are likely to need a catheter (tube) in your bladder to drain your urine. This is usually kept in until you are able to walk to the toilet.
After the operation you should be:
- offered pain relief such as paracetamol and ibuprofen; you can ask for stronger pain relief if you need it
- advised to take a course of antibiotics to reduce the risk of infection
- advised to take laxatives to make it easier and more comfortable to open your bowels
- offered an appointment with a physiotherapist; this may be while you are in hospital or at a follow-up appointment.
Rarely, women require another operation to repair the tear. You should seek advice from your healthcare professional at any point if you are worried about the way your tear is healing.
Will I be able to breastfeed?
Yes. None of the treatments offered will prevent you from breastfeeding. However, some women find it difficult to sit down for long periods of time. Breastfeeding in positions other than sitting, or using ice packs on your perineum, may be helpful. If you feel that you need additional support, you should speak to your healthcare professional as there may be specialist breastfeeding services in your area.
What can help me recover?
Keep your perineum clean. Wash daily using water only. Do not use any products on the area. Change your sanitary pads regularly. Wash your hands before and after going to the toilet. These measures will reduce the risk of infection in the stitches.
What do I need to know about my stitches?
You will have stitches between your vagina and anus and also beneath your skin. They will eventually all dissolve (soften and fall out) and you may notice small threads in your pad or in the bath. You may be able to feel some of the stitches, especially those around the anus muscle, for up to 3 months.
After having any tear, you are likely to experience pain or soreness for 4–6 weeks after giving birth, particularly when walking or sitting. The stitches can irritate as healing takes place, but this is normal. Passing urine can cause stinging – pouring water over the area when urinating can help.
If you are worried about the way your wound is healing or if you notice any bleeding from the tear, any smell or any increase in pain, you should see your healthcare professional. This might be a sign of infection and you may need some antibiotics to help it heal.
What do I need to know about my bowels?
Opening your bowels should not affect your stitches. For the first few days after your third- or fourthdegree tear is repaired, control of your bowels may not be as good as before you had your baby. It is important to eat well and drink plenty of water to help avoid constipation. You should drink at least 2 litres of water every day and eat a healthy balanced diet (for instance fruit, vegetables, cereals and wholemeal bread).
When opening your bowels, the best position to sit in is with your feet on a stool to raise your knees above your hips (see image). This helps straighten out your bowels. Try to relax and rest your elbows on your knees. Bulge out your tummy by taking big abdominal breaths – this will help to expel your faeces without straining. Take your time and do not rush.
How can I improve my bladder and bowel control?
It is important to do pelvic floor exercises as soon as you can after birth. This strengthens the muscles around the vagina and anus and helps healing. Your pelvic floor muscles will not be very strong straight after giving birth. The image shows a side view of your pelvic floor muscles.
You may feel that initially you have very little sensation in your pelvic floor, but this should improve the more you do your exercises. If the sensation does not improve, you may need further treatment such as physiotherapy, particularly if you experience any bladder or bowel incontinence. Physiotherapy will include teaching you how to correctly squeeze and strengthen your anal sphincter muscles to help reduce incontinence.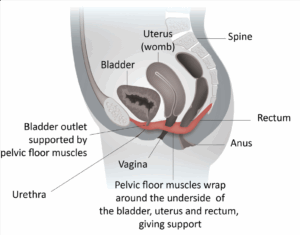
What is anal incontinence?
Anal incontinence is when you have problems controlling your bowels. Symptoms include sudden, uncontrollable urges to open your bowels and not being able to control passing wind. You may also soil yourself or leak faeces. Most third- or fourth-degree tears heal completely, but some women may experience these symptoms. It is important to talk about any concerns you have. Women with anal incontinence will be referred to a specialist team for treatment, which may include physiotherapy or surgery.
What should I expect when getting back to normal daily activities?
Every woman’s recovery will be slightly different, and what they view as normal daily activities will also differ. If you have had a third- or fourth-degree tear, you should avoid strenuous activity or heavy lifting for 4–6 weeks. After 4–6 weeks, you can gradually increase your general activity.
Looking after a newborn baby and recovering from an operation for a perineal tear can be hard. Support from family and friends can really help you while your body gradually adjusts and gets better. If you continue to experience symptoms after 6 months, see your healthcare professional.
Experiencing complications when giving birth can be very distressing and disturbing, and for some women there is a risk of post-traumatic stress disorder (PTSD). Following a perineal tear, if you are developing anxiety, have low mood or feel that you need additional support, you should talk to your healthcare professional.
When can I have sex?
Many women are worried by the thought of having sexual intercourse again after they have given birth, particularly when they have experienced a third- or fourth-degree tear. Once your stitches have healed and bleeding has stopped, you can have sex again when it feels right for you and your partner.
It is important that you choose and use a suitable method of contraception as it is possible to get pregnant very soon after giving birth, even before you have a period. You can discuss your contraception options with your healthcare professional.
Perineal massage, either on your own or with your partner, may help you feel more comfortable before you begin having sex again. You may notice your vagina feels drier than usual, particularly if you are breastfeeding. A water-soluble lubricant may be helpful.
Sex may be uncomfortable and feel different at first but the discomfort should not persist. You and your partner may be anxious and talking about these feelings may help, as it is important that you both feel ready and relaxed. If you continue to experience pain or discomfort, you should raise these concerns with your healthcare professional.
What follow-up arrangements should I expect?
You may be offered a follow-up appointment at the hospital 6–12 weeks after you have had your baby to check that your wound is healing properly. You will be asked questions about whether you have any problems controlling your bowels. You may be referred to a specialist if you do. You will also have the opportunity to discuss the birth and any concerns that you may have.
What about my future birth plans?
If you have recovered well and do not have any symptoms, you may wish to consider a vaginal birth. If you continue to experience symptoms from the third- or fourth-degree tear, you may prefer to consider a planned caesarean birth.
Currently, there is limited evidence as to whether or not you are at increased risk of having another third- or fourth-degree tear. It is suggested that women who have had a third- or fourth-degree tear in their first birth have a 7 to 10 in 100 chance of having a similar tear in their next vaginal birth. Risk factors for having a repeat third- or fourth-degree tear include having a forceps birth, your baby being born heavier than 4 kg and being of Asian ethnicity.
You will be able to discuss your options for future births at your follow-up appointment or early in your next pregnancy. Your healthcare professional will explore your individual experience and preferences so that you can make the decision that is right for you.
Making a choice
Further information and support
RCOG perineal tears hub: www.rcog.org.uk/tears
Mothers with Anal Sphincter Injuries in Childbirth (MASIC): https://masic.org.uk
Birth Trauma Association: www.birthtraumaassociation.org.uk
Bladder and Bowel Community: www.bladderandbowel.org
