Birth Options After Previous Caesarean Section
Please note, this page is printable by selecting the normal print options on your computer.
This information is for you if you have had one caesarean section and want to know more about your birth options when having another baby. It may also be helpful if you are a relative or friend of someone who is in this situation.
How common is it to have a caesarean section?
More than one in five women in the UK currently give birth by caesarean section. About half of these are as a planned operation and the other half are as an emergency. Many women have more than one caesarean section.
What are my choices for birth after one caesarean section?
If you have had a caesarean section, you may be thinking about how to give birth next time. Planning for a vaginal birth after caesarean (VBAC) or choosing an elective repeat caesarean section (ERCS) have different benefits and risks.
In considering your options, your previous pregnancies and medical history are important factors to take into account, including:
- the reason you had your caesarean section
- whether you have had a previous vaginal birth
- whether there were any complications at the time or during your recovery
- the type of cut that was made in your uterus (womb)
- how you felt about your previous birth
- whether your current pregnancy has been straightforward or whether there have been any problems or complications
- how many more babies you are hoping to have in future; the risks increase with each caesarean section, so if you plan to have more babies it may be better to try to avoid another caesarean section if possible.
To help you decide, your healthcare professionals will discuss your birth options with you at your antenatal visit, ideally before 28 weeks.
What if I have had more than one caesarean section?
If you are considering a vaginal birth but have had more than one caesarean section delivery, you should have a detailed discussion with a senior obstetrician about the potential risks, benefits and success rate in your individual situation.
What is VBAC?
VBAC stands for ‘vaginal birth after caesarean’. It is the term used when a woman gives birth vaginally, having had a caesarean section in the past. Vaginal birth includes normal delivery and birth assisted by forceps or ventouse (vacuum cup).
What is an ERCS?
ERCS stands for ‘elective (planned) repeat caesarean section’. You will usually have the operation after 39 weeks of pregnancy. This is because babies born by caesarean section earlier than this are more likely to need to be admitted to the special care baby unit for help with their breathing.
What are my chances of a successful VBAC?
After one caesarean section, about three out of four women with a straightforward pregnancy who go into labour naturally give birth vaginally.
A number of factors make a successful vaginal birth more likely, including:
- previous vaginal birth, particularly if you have had previous successful VBAC; if you have had a vaginal birth, either before or after your caesarean section, about 8–9 out of 10 women can have another vaginal birth
- your labour starting naturally
- your body mass index (BMI) at booking being less than 30.
What are the advantages of a successful VBAC?
Successful VBAC has fewer complications than ERCS. If you do have a successful vaginal birth:
- you will have a greater chance of a vaginal birth in future pregnancies
- your recovery is likely to be quicker, you should be able to get back to everyday activities more quickly and you should be able to drive sooner
- your stay in hospital may be shorter
- you are more likely to be able to have skin-to-skin contact with your baby immediately after birth and to be able to breastfeed successfully
- you will avoid the risks of an operation
- your baby will have less chance of initial breathing problems.
What are the disadvantages of VBAC?
- You may need to have an emergency caesarean section during labour. This happens in 25 out of 100 women. This is only slightly higher than if you were labouring for the first time, when the chance of an emergency caesarean section is 20 in 100 women. An emergency caesarean section carries more risks than a planned caesarean section. The most common reasons for an emergency caesarean section are if your labour slows or if there is a concern for the wellbeing of your baby.
- You have a slightly higher chance of needing a blood transfusion compared with women who choose a planned second caesarean section. The scar on your uterus may separate and/or tear (rupture). This can occur in 1 in 200 women. This risk increases by 2 to 3 times if your labour is induced. If there are warning signs of these complications, your baby will be delivered by emergency caesarean section. Serious consequences for you and your baby are rare.
- Serious risk to your baby such as brain injury or stillbirth is higher than for a planned caesarean section but is the same as if you were labouring for the first time.
- You may need an assisted vaginal birth using ventouse or forceps. See the RCOG patient information An assisted vaginal birth (ventouse or forceps) (rcog.org.uk/en/patients/patientleaflets/assisted-vaginal-birth-ventouse-or-forceps).
- You may experience a tear involving the muscle that controls the anus or rectum (third or fourth degree tear). See the RCOG patient information A third- or fourth-degree tear during birth (rcog.org.uk/en/patients/patient-leaflets/third–or-fourth-degree-tear-during-childbirth) for more information.
When is VBAC not advisable?
VBAC is normally an option for most women but it is not advisable when:
- you have had three or more previous caesarean deliveries
- your uterus has ruptured during a previous labour
- your previous caesarean section was ‘classical’, i.e. where the incision involved the upper part of the uterus
- you have other pregnancy complications that require a planned caesarean section.
What are the advantages of ERCS?
- There is a smaller risk of uterine scar rupture (1 in 1000).
- It avoids the risks of labour and the rare serious risks to your baby (2 in 1000).
- You will know the date of planned birth. However, 1 in 10 women go into labour before this date and sometimes this date may be changed for other reasons.
What are the disadvantages of ERCS?
- A repeat caesarean section usually takes longer than the first operation because of scar tissue. Scar tissue may also make the operation more difficult and can result in damage to your bowel or bladder.
- You can get a wound infection that can take several weeks to heal.
- You may need a blood transfusion.
- You have a higher risk of developing a blood clot (thrombosis) in the legs (deep vein thrombosis) or lungs (pulmonary embolism). See the RCOG patient information Reducing the risk of venous thrombosis in pregnancy and after birth (rcog.org.uk/en/patients/patient-leaflets/reducing-therisk-of-venous-thrombosis-in-pregnancy-and-after-birth).
- You may have a longer recovery period and may need extra help at home. You will be unable to drive for about 6 weeks after surgery (check with your insurance company).
- You are more likely to need a planned caesarean section in future pregnancies. More scar tissue occurs with each caesarean section. This increases the possibility of the placenta growing into
the scar, making it difficult to remove during any future deliveries (placenta accreta or percreta). This can result in bleeding and may require a hysterectomy. All serious risks increase with every caesarean section you have.
- Your baby’s skin may be cut at the time of caesarean section. This happens in 2 out of every 100 babies delivered by caesarean section, but usually heals without any further harm.
- Breathing problems for your baby are quite common after caesarean section but usually do not last long. Between 4 and 5 in 100 babies born by planned caesarean section at or after 39 weeks have breathing problems compared with 2 to 3 in 100 following VBAC. There is a higher risk if you have a planned caesarean section earlier than 39 weeks (6 in 100 babies at 38 weeks).
What happens when I go into labour if I’m planning a VBAC?
You will be advised to give birth in hospital so that an emergency caesarean section can be carried out if necessary. Contact the hospital as soon as you think you have gone into labour or if your waters break.
Once you start having regular contractions, you will be advised to have your baby’s heartbeat monitored continuously during labour. This is to ensure your baby’s wellbeing, since changes in the heartbeat pattern can be an early sign of problems with your previous caesarean scar. You can choose various options for pain relief, including an epidural.
What happens if I do not go into labour when planning a VBAC?
If labour does not start by 41 completed weeks, your obstetrician will discuss your birth options again with you. These may include:
- continue to wait for labour to start naturally
- induction of labour; this can increase the risk of scar rupture and lowers the chance of a successful VBAC
What happens if I have an ERCS planned but I go into labour?
Let your maternity team know what is happening. It is likely that an emergency caesarean section will be offered once labour is confirmed. If labour is very advanced, it may be safer for you and your baby to have a vaginal birth. Your maternity team will discuss this with you.
Key points
- If you are fit and healthy, both VBAC and ERCS are safe choices with very small risks.
- 3 out of 4 women who have had one caesarean section and then have a straightforward pregnancy and go into labour naturally give birth vaginally.
- 9 out of 10 women will have a successful VBAC if they have ever given birth vaginally. Successful VBAC has the fewest complications.
- Giving birth vaginally carries small risks for you and your baby but, if you have a successful vaginal birth, future labours are less complicated with fewer risks for you and your baby.
- Having a caesarean section makes future births more complicated.
- Most women who have a planned caesarean section recover well and have healthy babies, but it takes longer to get back to normal after your baby is born.
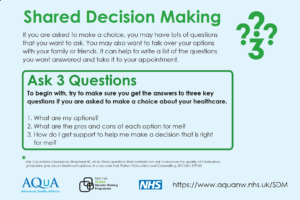
Making a choice
Further information
- NICE guidance on caesarean section: nice.org.uk/guidance/cg132
- RCOG patient information A third- or fourth-degree tear during birth: rcog.org.uk/en/patients/ patient-leaflets/third–or-fourth-degree-tear-during-childbirth
RCOG patient information An assisted vaginal birth (ventouse or forceps): www.rcog.org.uk/en/
